Until recently, iron infusions were strictly a hospital-only procedure, but they are now easy to do in general practice
Until recently, iron infusions were strictly a hospital-only procedure, but they are now easy to do in general practice
Jasmine is a 15-year-old girl with an obsession for crunching on ice, diagnosed with pica syndrome. Your investigations show that her Hb is low at 76g/L, and she is severely iron deficient. Should you refer Jasmine for a hospital admission for a six-hour iron infusion? Or can she be safely managed in your clinic with a 15-minute iron infusion administered by you and your clinical team?
Since the PBS listing of ferrous carboxymaltose (Ferinject) in August 2014, the world of iron therapy in general practice has opened up enormously. GPs are now able to investigate and treat iron deficiency on-site at their clinic.
Ferinject is a new, small-molecule form of intravenous iron and is a safe option to administer in a primary healthcare setting. Compared with the older versions of IV iron, it is also much quicker to administer. The twin advantages of safety and convenience have paved the way for IV iron administration in general practice to become the new normal.
Just as there’s a trend towards GPs having specific skills, such as excisions of skin cancers, IUD insertion and sports and travel medicine, we now have a growing cohort of GPs performing IV iron infusions.
For me, this has to be one of the most exciting aspects of IV iron treatment – allowing what was once an in-hospital procedure to be available in the community setting.
The PBS listing for ferrous carboxymaltose1 is a general benefit for 500mg in 10ml – two vials and one repeat. There are no restrictions or authority requirements. The cost to the PBS is $307 for two vials.
The product information for Ferinject states that it “is indicated for the treatment of iron deficiency when oral iron preparations are ineffective or cannot be used. The diagnosis must be based on laboratory tests”.
It is therefore vital to get a good handle on the diagnosis of iron deficiency before undertaking iron infusions of ferrous carboxymaltose in your practice. The diagnosis of the cause must also be established where possible. The sentinel article on iron deficiency is the 2010 MJA article Diagnosis and management of iron deficiency anaemia: a clinical update2 and is essential reading.
The BloodSafe eLearning website educational module provides an online learning module on iron deficiency anaemia3, which is free to access.
DIAGNOSIS
The textbook iron deficiency picture is of a low ferritin, low transferrin saturation and increased iron binding capacity, but the interpretation of iron studies can be challenging.
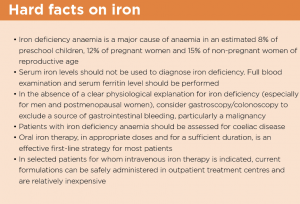
Serum iron alone is of little or no value due to significant diurnal variation2 and should not be used to diagnose iron deficiency. Ferritin should also be ordered when investigating iron deficiency. Ferritin below 15?g/L for adults and 12?g/L for children is diagnostic of iron deficiency.
Ferritin between 15-20?g/L (in children) and 15-30?g/L in adults is suggestive of low iron stores and may also warrant further clinical enquiry, especially regarding diet and menstrual status. However, ferritin is rarely used alone in clinical practice as many people at risk of iron deficiency may also have inflammatory conditions which may cause elevations in ferritin unrelated to iron status, as it is an acute phase reactant.
There is a non-Medicare funded test, soluble transferrin receptor (sTfR) concentration, which is raised in the presence of iron deficiency and is not affected by inflammation. This test can be difficult to access, but may become more widely used in the future.
If iron studies and FBC are difficult to interpret due to the coexistence of possible iron deficiency and chronic disease, then a phone call to your local pathology lab or a friendly haematologist can help to clarify the picture.
Deficiency causes include excessive blood loss, inadequate iron intake in the diet and inadequate iron absorption by the gut.
Excellent guidelines from the Gastroenterological Society of Australia on iron deficiency4 are worth reviewing, especially the section on investigation of the causes of iron deficiency.
Once iron deficiency has been diagnosed, it is imperative to establish its cause.
Iron deficiency is never a diagnosis in itself. The cause for the iron deficiency must be investigated and treated. Unless another cause is obvious, this will usually entail specialist gastroenterology referral for consideration and investigation of possible malabsorption or GI blood loss with upper and/or lower endoscopies as appropriate.
REPLACEMENT
It is acceptable to begin iron replacement therapy while the patient is undergoing investigation for the cause of their deficiency.
The waiting time for endoscopy/colonoscopy can take months, so it’s not necessary for patients to suffer from untreated iron deficiency while waiting. However, there’s a risk that an iron infusion will make the patient feel better, and they’ll fail to follow up with the required investigations. There would be nothing worse than a patient failing to attend for their colonoscopy because they feel better from the iron replacement, only to find out later that they have bowel cancer.
While GPs can help patients enormously by giving iron infusions in the community setting, oral iron remains the mainstay of iron replacement therapy. A working knowledge of oral iron supplements and brand names is essential. Many OTC preparations have tiny amounts of iron that are of no benefit in treating iron deficiency.
The best resources regarding oral iron are available on the Blood Safe website5 – it includes pictures of the recommended products, dosing regimens, as well as useful tips on reducing GI side effects. Remember: it takes three months of oral iron after the Hb has normalised to replenish iron stores. If a patient fails to respond to correctly administered oral iron, this should raise the red flag for a GI specialist referral and further investigation.
As we are all too well aware, some patients can’t tolerate oral iron. The gastrointestinal side effects can be quite severe, leading many patients to tolerate the symptoms of iron deficiency rather than take oral iron. This is one scenario where IV iron infusions come into play. A simple IV infusion over five to 15 minutes can offer the perfect solution.
PROCEDURE
At Chandlers Hill surgery in Adelaide, we have just completed two years of administering IV iron to more than 80 patients. As our confidence has increased, we have gone from an original 45-minute procedure to a system where our practice nurses administer the IV iron via a slow push over five to 15 minutes, depending on the dose.
The procedure starts with the GP consent protocol and an IV canula insertion by a GP or qualified nurse. There are two options for administering the IV iron – direct slow push of undiluted ferrous carboxymaltose, or an infusion (mixed with a 100ml saline) over 15 minutes. Both methods work well and you should choose whatever works best for your setting.
Keep in mind that some nurses may be anxious about iron infusions in general practice as they have experienced the old-style hospital-based infusions that went over many hours and required intensive monitoring. It is essential to make sure that your nurse colleagues are comfortable with the procedure and feel well supported.
The contraindications and precautions to iron infusion are listed in the PI sheet and are required reading. It is not approved for use in children under 14 or in the first trimester of pregnancy. Hypersensitivity to Ferinject, microcytic anaemia not due to iron deficiency, and iron overload are top of the contraindications list. Be cautious with atopic patients and those who show evidence of liver dysfunction and active infection.
A mandatory 30-minute supervised waiting period post-infusion is a compulsory requirement in case of an anaphylactic reaction. This is rare but potentially fatal, and can occur even if previous doses of IV iron have been well tolerated. You and your staff must be up to date with CPR skills and anaphylaxis management, and must have the appropriate resuscitation equipment on-site.
Paravenous leakage leading to a permanent brown stain on the skin is another potential complication. This can occur despite the best–practice insertion of the IV canula and administration of the iron infusion.
It is my standard practice to flush the IV canula with 10ml of saline before and after the infusion. Stop the infusion immediately if there’s any concern about leakage of the iron into the surrounding tissue. Be aware that the iron infusion is isotonic, so the patient will not feel any discomfort in the case of a leak.
Ferritin and iron should be measured six weeks post-infusion and monitored thereafter within the timeline relevant to the clinical scenario.
INDICATIONS
The list of indications for IV iron is growing, including the many clinical scenarios where oral iron is not well absorbed due to the action of a protein named hepcidin, a down- regulator of iron absorption. Due to the action of hepcidin, inflammatory states, post-operative anaemia and postpartum anaemia will not respond well to oral iron.
IV iron treatment is a perfect option in these clinical scenarios, with the standard hospital discharge process usually including a prescription for oral iron. The patient who has had a blood transfusion in a hospital setting may still have low iron stores and will not respond well to oral iron.
There is no need for a new mother to struggle with a baby and a chronically low iron when you can offer her an infusion of IV ferrous carboxymaltose at your clinic.
Heart failure is another common condition that improves clinically when IV iron is administered. You can help these patients enormously by maximising their red cell oxygen-carrying capability.
The new target for ferritin in these patients is 100?g/L (even though our pathology reports have 30?g/L as normal). My mantra is “100 is the new 30”. I have seen excellent rises in Hb when IV ferrous carboxymaltose was given to patients with heart failure. Often their anaemia had been put down to “chronic disease” but it pays to be vigilant and look out for iron deficiency.
The push for better management of blood transfusions – a precious resource always in short supply – has also seen a rise in the need to replenish iron stores before major surgery, such as joint replacements, gastrointestinal, cardiac and gynaecology surgery.
A 2010 South Australian study6 has clearly shown that preoperative iron deficiency anaemia was associated with a 49% chance of requiring a blood transfusion versus 22% for non-anaemic patients.
One could argue that a consideration of replenishing iron stores before an elective surgical procedure should be part of the assessment for surgery.
Iron infusions during pregnancy are not indicated in the first trimester of pregnancy, but this is a growing area of interest because we know that women with normal Hb and iron stores replete at the time of delivery are less likely to require blood transfusions postpartum than those with iron deficiency and anaemia.
Current South Australian guidelines require iron infusions during pregnancy to be performed in an inpatient setting in order to reduce the risk of anaphylaxis and harm to the fetus and mother. Your local antenatal service will provide you with up-to-date protocols around iron infusions in pregnancy.
There are also complex algorithms around replenishing iron in patients with chronic renal failure who are on EPO and/or having dialysis, but these are beyond the scope of this article.
Don’t be surprised if a CRF patient of yours with anaemia and a ferritin of 250 is given IV iron by the renal team. Most renal centres in Australia are managing iron replacement very well.
Dr Daniel Byrne is a general practitioner working in Adelaide and has been involved in GP hospital liaison and eHealth for over 20 years
References:
1 http://www.pbs.gov.au/medicine/item/10104T
2 https://www.mja.com.au/journal/2010/193/9/diagnosis-and-management-iron-deficiency-anaemia-clinical-update
3 https://bloodsafelearning.org.au/course/iron-deficiency-anaemia-ida/
4 http://www.gesa.org.au/files/editor_upload/File/Professional/Iron%20Deficiency%202015.pdf
5 http://www.sahealth.sa.gov.au/bloodsafe – and follow links to “oral dosing guide for clinicians”
6http://www.sahealth.sa.gov.au/wpswcmconnect/04f811004f8740ed98b0dbc4163822ed/GapAnalysisPreopAnaemiaRatesSurgicalPatientsSAHosp-BloodSafe.pdf?MOD=AJPERCACHEID=04f811004f8740ed98b0d