Pregnancy can present an opportunity for establishing healthier eating habits, not only for the mum-to-be
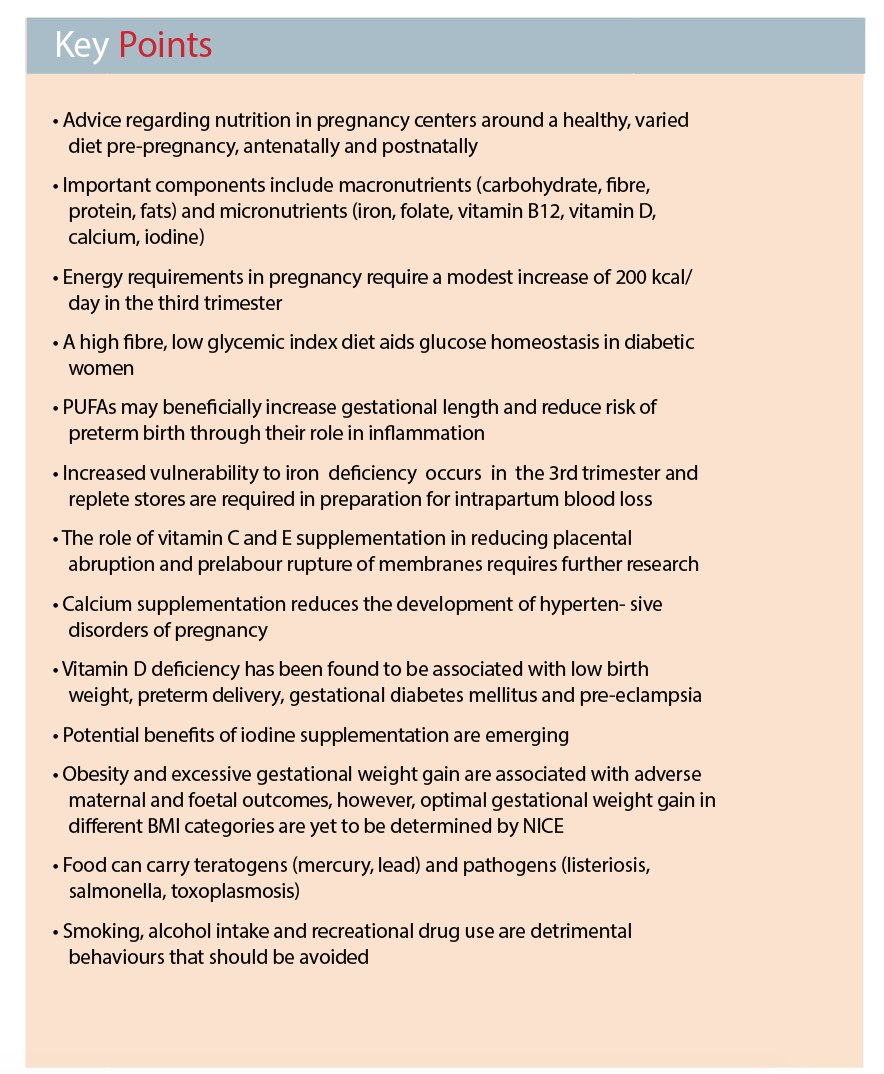
The pivotal role of nutrition in pregnancy is well established, and has important implications on subsequent maternal and offspring health. Optimal nutrition around conception and maintained throughout pregnancy promotes optimal fetal growth and development.
Growth trajectories in utero and size at birth are related to the offspring’s risk of developing disease in later life, especially chronic non-communicable diseases such as hypertension, diabetes and coronary heart disease (the Barker hypothesis).
The fetus relies on maternal nutrition for growth and development. Additionally, nutrition forms the basis of maternal well-being and equips the mother for delivery and postnatal recovery. Optimal nutritional intake also has the potential to reduce complications, such as gestational diabetes and pre-eclampsia, and their associated short and long-term effects.
Pregnancy is an opportunity to help parents establish healthy dietary habits that can potentially be adopted by their family, establishing a beneficial background to optimal health for future generations.

Maternal and fetal circulations
The placenta links the maternal and fetal circulations, with syncytiotrophoblasts lining placental villi and consisting of two polarised membranes: the microvillous membrane facing the maternal circulation, and basal plasma membrane facing the fetal capillary epithelium.
Thus, nutrients must pass through these two membranes before crossing the fetal capillary epithelium to enter the fetal circulation. The expression and activity of transporter mechanisms within the placental-fetal unit have been found to be associated with fetal growth restriction, macrosomia, diabetes, obesity and maternal nutrient availability.
Energy and macronutrients
Energy requirements in pregnancy vary between individuals, and guidelines differ between countries, however, it is agreed that additional requirements are relatively small.
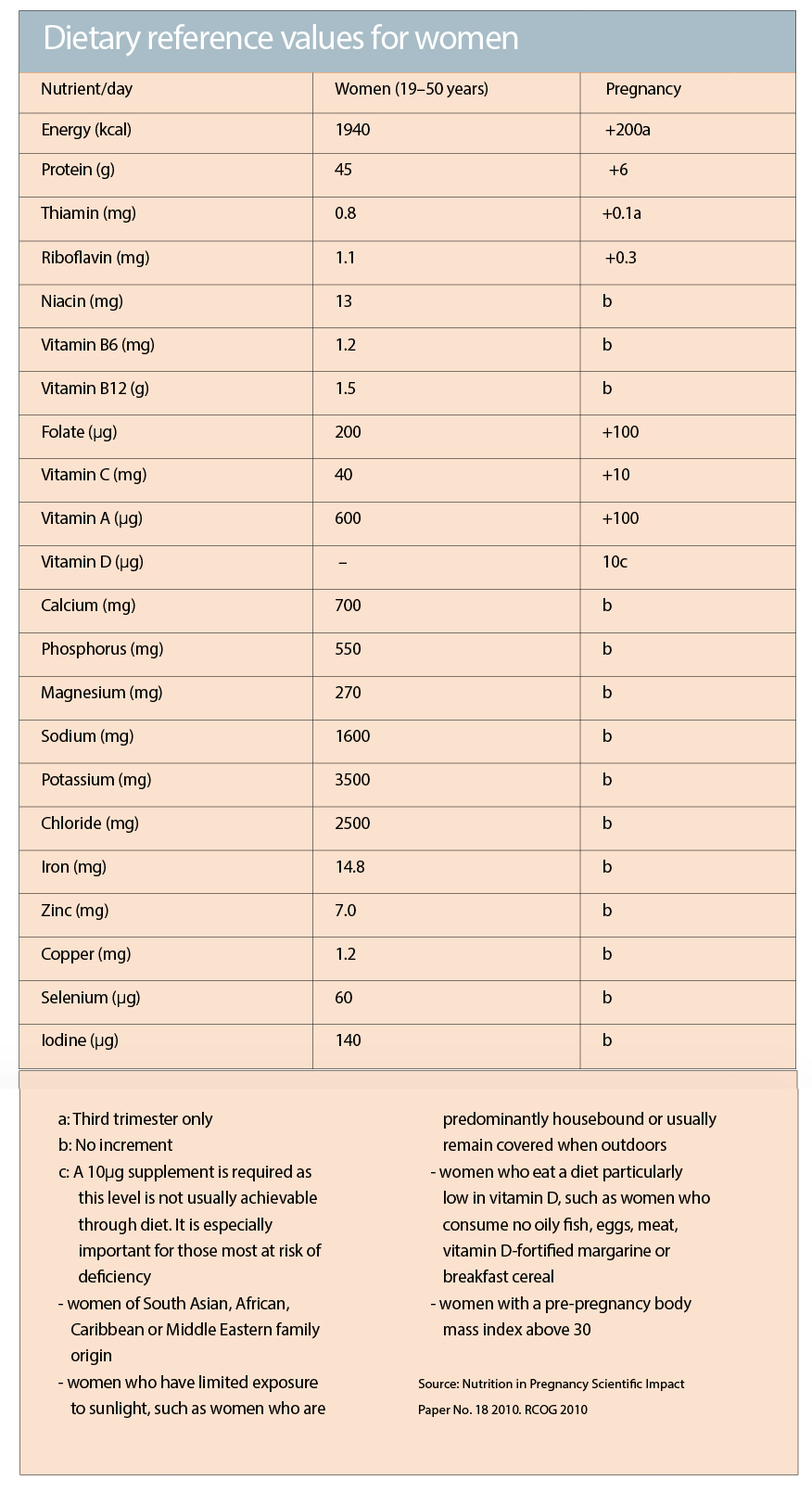
The Royal College of Obstetricians and Gynaecologists (ROCG) recommends a modest increase of 200 kcal/day in the third trimester an approximate 10% increase from the 1940 kcal/day recommendation in a non-pregnant adult woman.
Calorie restriction is not advised during pregnancy, and dietary recommendations focus on achieving and maintaining a healthy weight over this period by basing meals on starchy foods (wholegrain if possible), eating fibre-rich foods, and consuming at least five portions a day of fruit and vegetables. Food high in fat and sugar (including fried food, sugary drinks and confectionery) should be avoided. Pregnant women are also advised to eat breakfast and to ensure that portion sizes and frequency of meals do not increase.
The ROCG advises low-fat dairy foods as a source of calcium, with a daily intake of protein in the form of lean meat, two portions of fish a week (one of which should be oily) or lentils, beans and tofu.
Carbohydrates and fibre:
Carbohydrates form the main substrate for foetal growth, fuelling maternal and fetal organ function and biosynthesis. Additionally, carbohydrates are used in the formation of structural components of cells, coenzymes and DNA. Maternal and fetal brain functions use glucose from carbohydrate as their preferred source of energy, with glucose providing at least 75% of foetal energy requirements. Glucose crosses the placenta by facilitated diffusion along a concentration gradient through members of the glucose transporter family.
Carbohydrate type and quantity can affect glucose homeostasis via release of insulin. The glycaemic index (GI) refers to the area under the curve for blood glucose concentrations during a two hour period after consuming a test food. A low GI suggests slower rates of digestion and absorption of the food’s carbohydrate, potentially relating to a lower insulin demand. It is therefore a modifiable macronutrient in the management of diabetes mellitus (gestational, type 1 and type 2), however, there is no evidence to support a low glycaemic index diet for healthy pregnant women.
Fibre affects the postprandial insulin response by influencing the accessibility of carbohydrates and nutrients to digestive enzymes, thus delaying their absorption. Fibre supports maternal digestive health, providing bulk to stool and absorbing water to aid transit time. This is especially beneficial as progesterone levels in pregnancy can result in constipation by increasing relaxation of intestinal smooth muscle.
Protein: Protein forms the building blocks for both structural and functional components of cells. Requirements are highest during the second and third trimesters due to the increased development and growth of both maternal and fetal tissue. Protein will also be used as an alternative energy source when carbohydrate intake is insufficient, therefore adequate carbohydrate intake is required in order for the protein to be used to allow cell synthesis to continue. Low socioeconomic status and women with limited dietary variety are at risk of suboptimal protein intake.
Plasma concentrations of most amino acids are higher in the fetal circulation. Over 15 different amino acid transporters mediate their transport against a concentration gradient.
Systems include the sodium dependent System A for small neutral amino acids, and the sodium independent System L for large neutral amino acids with branched or bulky side chains.
Fats and essential fatty acids: Fat aids transport of fat-soluble vitamins A, K, D and E and are required for structural (e.g. membrane lipids) and metabolic functions (e.g. precursor for steroid hormones).
Polyunsaturated fatty acids (PUFAs) are important for neurological development including the foetal brain, nervous system and retina. Oily fish, nuts, seeds, vegetable oils, margarines and green leafy vegetables are encouraged to obtain a greater intake of PUFAs.
Essential fatty acids, linoleic and alpha linolenic acid, are precursors for n-6, n-3 long-chain polyunsaturated fatty acids (LC-PUFA) and prostaglandins; these are components of the inflammatory process with a role in diseases characterised by inflammation, reproductive health, cervical ripening and initiation of labour.
Systematic reviews have found little or no effect of n-3 LCPUFA supplementation in pregnancy on cognitive development, birth weight, gestational diabetes mellitus or pre-eclampsia. There is, however, a beneficial effect on gestational length and lowering the risk of preterm birth.
Placental triglyceride lipases break down triglycerides into fatty acids. Fatty acids and ketone bodies, produced by maternal lipolysis, cross the placenta by diffusion. Cholesterol-carrying lipoproteins LDL, HDL and VLDL transport cholesterol into the fetal circulation. Syncytiotrophoblasts express lipoprotein receptors and lipid transporters in the foetal endothelium allow cholesterol to enter the fetal circulation. The fetus also synthesises cholesterol endogenously.
Micronutrients
Iron and vitamin C: Iron is required for foetal development, placental growth and expansion of maternal red blood cell mass. Especially in late pregnancy, maternal vulnerability to iron deficiency occurs as iron transfer to the fetus takes priority in order to meet increased demand. Iron deficiency has been associated with a higher risk of preterm delivery, low birth weight, infant iron deficiency and long-term cognition and brain function. Replete stores are required in preparation for childbirth as significant blood loss may occur intrapartum. Iron transfer to the fetus is facilitated through placental transferrin receptors for endocytosis of transferrin-bound iron. Vitamin C aids iron absorption and competes for placental receptors with glucose, however maternal hyperglycaemia does not result in fetal hypovitaminosis C.
A recent Cochrane review suggests vitamin C might play a role in preventing placental abruption and premature rupture of membranes. The risk of stillbirth, neonatal death, IUGR and pre-eclampsia were not affected by vitamin C supplementation. However, women supplemented with vitamin C alone or in combination with other supplements were more likely to self-report side effects such as abdominal pain. Fewer pre-term births were seen in these women.
Folate and vitamin B12: The use of peri-conceptional folic acid to prevent neural tube defects is well established, however it has no clear effect on cleft palate/lip or congenital cardiovascular defects. Five percent of the general population has marginal to severe folate deficiency and therefore all women are advised to take 400 µg/day folic acid prior to conception until the 13th week of pregnancy with higher doses in certain circumstances (see table below). Vitamin B12 is transported via placental receptors. Both micronutrients are associated with a reduction in megaloblastic anaemia, placental vascular disorders, preterm birth, low birth weight and also in the numbers of babies small for their gestational age, via regulation of circulating homocysteine levels.
Homocysteine levels are influenced by the activity of methylene tetrahydrofolate reductase (MTHFR). The genetic variant, C6777T leads to impaired MTHFR function and its presence is associated with an increased risk for pre-eclampsia and recurrent pregnancy loss, potentially via elevated homocysteine levels. Low dietary intake of folic acid can exacerbate this but evidence is lacking with regard to whether pregnant women carrying the C6777T variant should take a higher folic acid supplement.
Vitamin D and calcium: Vitamin D is required for immune and nervous system function and mediates the accumulation of fetal calcium from maternal stores in skeletal growth. Vitamin D deficiency can result in rickets, craniotabes and osteopenia. Calcium supplementation reduces the development of hypertensive disorders of pregnancy and an increasing body of evidence demonstrates a relationship between vitamin D deficiency and low birth weight, preterm delivery, gestational diabetes mellitus and pre-eclampsia. Individuals particularly at risk for vitamin D deficiency include those of South Asian, African, Caribbean or Middle Eastern origin, a body mass index >30, and low sun exposure.
Iodine: Iodine is required for fetal thyroid function and neurological development. Iodine deficiency has been linked with cognitive deficits. Peri-conceptional and antenatal supplementation in regions of severe iodine deficiency have been found to reduce the risk of cretinism and improve motor function. Reports of gestational iodine deficiency and potential benefits of iodine supplementation are emerging.
Vitamin E: More evidence regarding vitamin E supplementation in pregnancy is required, as a recent Cochrane review suggested an advantageous role in reducing the risk of placental abruption. However, supplementation with vitamin E was associated with an increased risk of self-reported abdominal pain and term prelabour rupture of membranes. There was no difference in vitamin E supplementation on the risk of stillbirth, preeclampsia, preterm birth and intrauterine growth retardation.
Weight gain and obesity
To achieve appropriate gestational weight gain, multiple factors must be balanced. These include calorific intake, level of physical activity, pre-pregnancy weight, age, nutritional status, percentage of body fat to fat free mass and basal metabolic rate.
A consideration must also be given to the increasing energy expenditure as the pregnancy progresses to support growth and development of the placental-fetal unit.
The relationship between gestational weight gain and pregnancy outcome is difficult to establish, as it reflects multiple components: fetus, placenta, uterus, amniotic fluid, maternal adipose tissue, blood volume expansion and enlargement of the mammary glands.
A high pre-pregnancy BMI carries adverse maternal and foetal outcomes – gestational diabetes mellitus, preeclampsia, caesarean section, assisted delivery, postpartum haemorrhage, infection and thrombosis, large for gestational age, birth defects and stillbirth. Periconceptionally and antenatally, these women should be warned of their increased risks, and encouraged to make lifestyle changes to support weight management. Randomised controlled trials of physical activity and dietary intervention in obese women have failed to demonstrate an effect on the risk of gestational diabetes and large for gestational age.
Special considerations
Smoking, alcohol and caffeine consumption and recreational drug use can have a detrimental effect on foetal nutrition, growth and development. Physical activity is beneficial by managing weight gain, preparing for labour and aiding glucose homeostasis, especially in diabetic women. Pregnant women are also at risk of food borne illness e.g. listeriosis in unpasteurised milk, cheese or pate, salmonella in partially cooked eggs, poultry and shellfish, and toxoplasmosis in undercooked meat or salad vegetables contaminated with soil or cat faeces. Methylmercury in fish is teratogenic, affecting development of the fetal nervous system, and should be restricted to two portions a week. Eating high levels of vitamin A is also teratogenic and therefore multi-vitamins containing vitamin A, liver, pate, fish liver oils and other food fortified with vitamin A should be avoided.
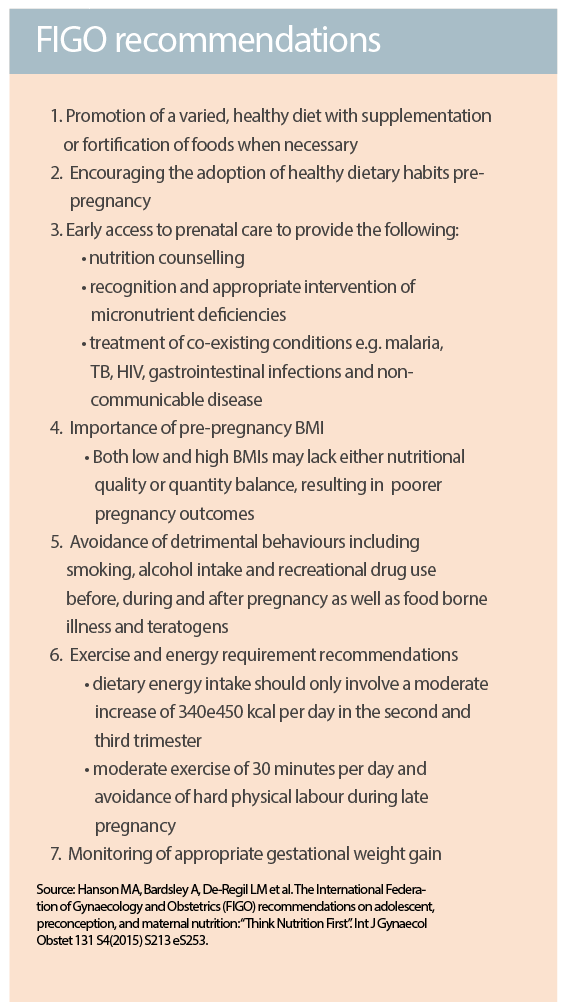
Nutrition in pregnancy requires a careful balance of both quality and quantity of intake in order to optimise fetal growth and development in addition to reducing maternal morbidity. Recommendations centre around early intervention through healthcare promotion of a varied, healthy diet, beneficial lifestyle behaviours and the use of supplementation or fortified foods as necessary. Such changes are also valuable if carried out in the long term by both the parents.
Dharmintra Pasupathy is a consultant/senior lecturer in Maternal and Fetal Medicine and Perinatal Epidemiology at the Women’s Health Academic Centre, Kings College, London
References available on request