The number of skin excision items have been reduced from 48 to 21, so there’s a lot to learn
Significant changes to MBS rebates for skin services have been introduced, including a new method to measure skin excisions and tighter restrictions on skin-flap repairs.
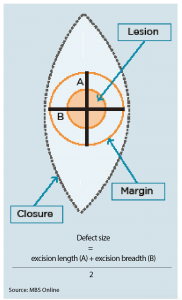
For items 31356 to 31376, which cover definitive surgical excisions with curative intent, necessary excision diameter (or defect size) must be calculated to determine which item number can be claimed.
The defect size is now calculated by the average of the width and the length of the lesion and an appropriate margin (see diagram).
Measurements should be taken before excision, and margin size determined in line with NHMRC guidelines.
Under the changes, which came into effect on November 1, doctors also need to retain histological reports and photographic or other supporting evidence that include scale.
It was a logical move, according to Associate Professor Stephen Shumack, of the Australasian College of Dermatologists.
“Obviously if you’ve got a bigger defect size, it’s going to be more difficult to repair that defect,” he said. “So it’s only reasonable that those item numbers reflect that degree of difficulty.”
In 2012, the government launched a review into skin services under the MBS after requests from the AMA and plastic surgeons group to rearrange and simplify items covering skin lesions and flap repairs.
The review indicated “inappropriate, low-quality and unnecessary skin-flap repair” were sometimes used instead of more appropriate direct suture closures, a spokesperson for the health department said.
Under the new MBS item numbers, doctors can no longer claim for some skin-flap repairs when small lesions are excised from areas such as the trunk.
“If you cut something out which is relatively small from back, the expectation is that you’ll close that or repair that without undertaking a skin-flap repair,” Professor Shumack said.
“There have been a fair number of skin flaps used to close relatively small defects on the trunk, and while some of these may well be justified, it was thought by this committee that most of these can probably be better closed and much more cheaply closed by primary closure rather than taking a skin-flap repair,” he told The Medical Republic.
While the implementation of the new item numbers had been “a bit of a hodgepodge”, with the actual update only publicised days before the implementation, it should make things much simpler for doctors, Professor Shumack said.
Under the changes, the 48 previous skin-excision items have now been reduced to 21.
“I think they will provide a more simplified way of organising billing and rebates for our patients, and I think this is only going to be good for our patient population,” he said.
“And it’s going to be much easier for Medicare to understand what sort of procedures and processes are being undertaken out there in clinical practice.”
There had always been higher rebates and different item numbers for “difficult areas” such as eyelids, ear, nose, lip, digits and genitalia, said Sydney GP Dr Gunninder Soin.
While these remain unchanged, now areas such as the scalp, whole of neck and lower leg are now in the second highest of three tiers of billing.
Five new item numbers have also been created for biopsy or excision of lesions from mucous membranes, and another two items have been changed to distinguish the biopsy or excision of lesions of mucous membranes from existing items.
At the same time, the government has added two new MRI services for women with metastatic breast cancer.
One service is for breast MRI where the patient has been diagnosed with metastatic cancer restricted to the regional lymph nodes, but the primary is undetectable by examination and conventional imaging.
The other service is MRI-guided biopsy where the patient has a suspicious lesion on MRI but not on conventional imaging.
“Breast MRI is a very, very sensitive test for assessing extent of disease and it can change management in around 10% of patients,” said breast radiologist Dr Michelle Reintals, chair of the Breast Imaging Reference Group.
But the rebates certainly don’t go far enough, she said.
“Best practice is that breast MRI is for women that require it, not based on strict eligibility criteria deemed by non-clinicians.”
Other personal risk factors, family history and type of cancer were also factors that needed to be considered, Dr Reintals said.