There is ongoing debate on the pros and cons of sudden cardiac death screening. Here’s the latest thinking
A longstanding patient brings his 18-year-old son, who has just been selected to play in a first-grade rugby team, to see you. He requests an ECG, because he has heard this is done in the United States. His team has no policy on ECG screening of their athletes. How would you manage this case?
Regular participation in sporting activity has long been encouraged to promote cardiovascular health, improve fitness and mobility, reduce obesity and to improve mental health. However, despite the overall benefits of exercise, occasionally we hear of tragic cases of young fit athletes, in the prime of their lives, succumbing to sudden cardiac death (SCD) while participating in their sport.
Sudden cardiac death is thought to affect approximately one in 200,000 athletes annually in the developed world, though this is likely to be an underestimate due to several factors. These include a lack of registry data, difficulty identifying causes in post mortem examinations, and an inability to identify the cause.
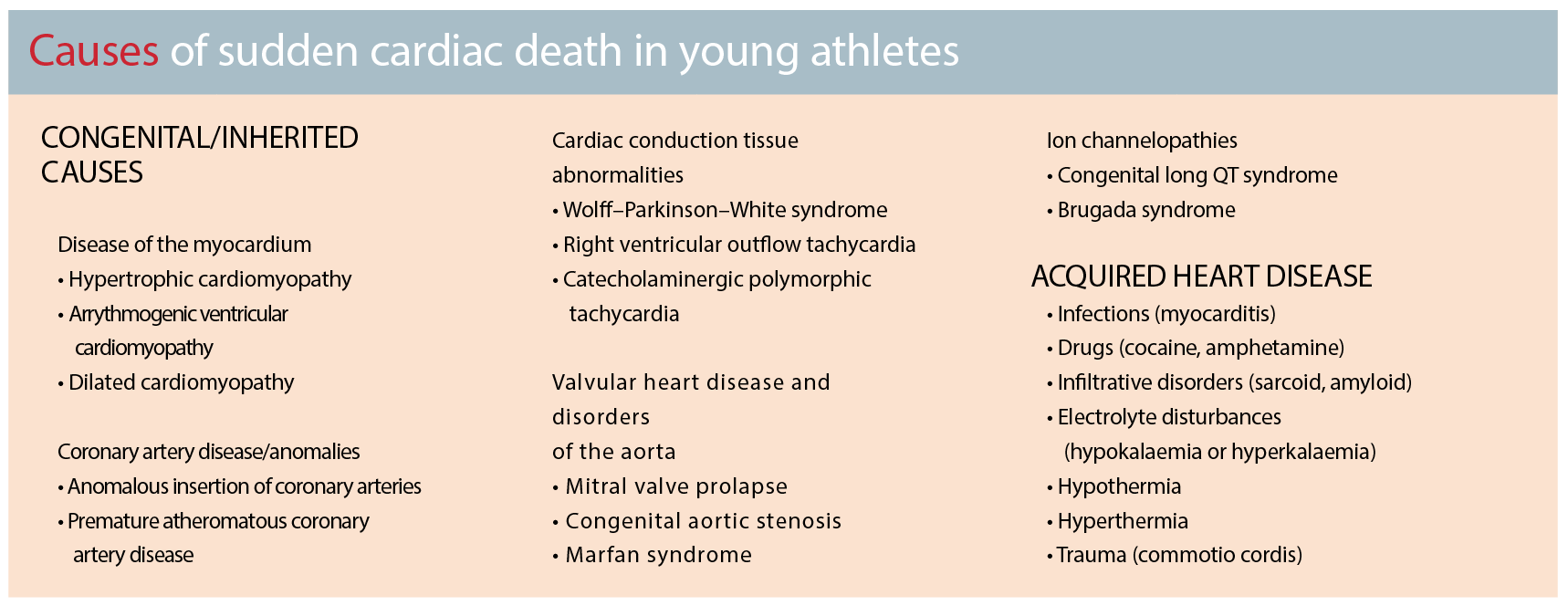
Causes
The majority of patients with cardiac diseases which are thought to increase the risk of sudden cardiac death are limited from performing strenuous physical activity due to symptoms and functional limitations. However, a small proportion will have no such limitations and remain asymptomatic while participating in competitive sport at the highest level. It is these athletes who are at risk of sudden cardiac death.
This is exemplified by cases such as those of Mark Vivian Foe, the Cameroon footballer who played for several seasons in the English Premier League and died from sudden cardiac death during an international game in 2003, as well as the death of a club runner in the London Marathon in 2005 who had run 19 marathons previously in under 3.5 hours. Until they suffered their fatal cardiac events, they had been asymptomatic with no previous cardiac disease diagnosed.
It is not proven that ECG screening alone prevents sudden cardiac death.
Most cases of sudden cardiac death in young athletes are related to underlying inherited cardiomyopathies, particularly hypertrophic cardiomyopathy (HCM), idiopathic left ventricular hypertrophy, and arrythmogenic ventricular cardiomyopathy. (see box page 38)
The second leading cause is coronary artery anomalies, particularly when the left main coronary artery arises from the right sinus of Valsalva – the acute angle of this insertion is thought to become prone to diminished blood flow as the aorta enlarges with exercise. Most patients with these abnormalities are asymptomatic prior to the fatal event and will likely have normal ECGs and two thirds may even have normal stress ECG results.
Other less common causes include electrophysiological abnormalities (eg Wolff-Parkinson White syndrome and long QT syndrome) or acquired causes such as myocarditis, drug use (eg. cocaine, amphetamines), electrolyte disturbances or significant hypo/hyperthermia. Sudden cardiac death may also be associated with direct trauma to an otherwise normal heart with a direct blow to the chest (commotio cordis).
Can we predict who is at risk?
There has been ongoing debate as to the pros and cons of screening for risk factors for sudden cardiac death in athletes. The primary goal of screening competitive athletes for sports participation is to identify or raise suspicion of cardiovascular abnormalities that are potentially responsible for sudden cardiac death on the athletic field to guide prevention strategies or treatments.
However, screening is problematic due to the low numbers of participants with underlying undiagnosed cardiac disease and the difficulties in detecting these risk factors. Most people with the disorders that increase one’s risk of sudden death will never have symptoms, even while engaging in physical activity. In addition, there is no ideal single test that can detect all potential underlying triggers.
Basic auscultation of the heart is likely to play a limited role, but will help identify athletes with underlying valvular abnormalities such as aortic stenosis, and up to 25% of those with hypertrophic cardiomyopathy. A 12-lead ECG can identify up to 63% of athletes who may be vulnerable to sudden cardiac death. This is of fundamental importance, as up to 80% of athletes who suffer sudden cardiac death have had no antecedent symptoms or family history.
As previously stated, one of the single most common causes of non-traumatic sudden cardiac death is HCM, an autosomal dominant disorder linked to several genetic mutations involving the cardiac sarcomere. The risks associated with hypertrophic cardiomyopathy are related to an increased risk for ventricular tachyarrhythmias, and most athletes with hypertrophic cardiomyopathy have an abnormal ECG.
Other diagnoses that may be picked up on ECG include arrhythmogenic right ventricular hypertrophy, long QT syndrome, Brugada syndrome, ventricular pre-excitation and left bundle branch block as a marker for cardiomyopathy.
However, many diseases that cause sudden death in athletes cannot be detected by an ECG. These include myocarditis, aortic disease, sudden arrhythmic death syndrome, catecholaminergic polymorphic VT, left ventricular non-compaction and anomalous origin of the coronary arteries.
Is screening effective?
It is not proven that ECG screening alone prevents sudden cardiac death. There is a widely quoted Italian study3 which showed the reduction of sudden cardiac death with a pre-participation screening program including ECGs, but this trial has not yet been replicated. It may well be that ECG screening works in Italy due to the relatively high prevalence in that country of certain genetic forms of heart disease with particular reference to arrhythmogenic right ventricular cardiomyopathy. Subsequent Israeli2 and Japanese studies with similar aims have not shown the benefits.
ECG screening is further complicated by the finding that 12-lead ECG tracings in athletes differ significantly from those in non-athletes. Physiologic ECG abnormalities in athletes can overlap with potentially serious cardiac diseases, and efforts to differentiate between the two entities are ongoing.
Common changes
The extent of cardiac morphological and electrical changes in trained athletes varies with the athlete’s gender (more prevalent and significant in males), race (increased in those of African / Caribbean descent), fitness, and type of sport undertaken.
Participation in sports that require high endurance, such as cycling, cross-country skiing, and rowing/canoeing has been shown to be significantly associated with a higher rate and greater extent of physiological ECG changes such as sinus bradycardia and increase of QRS voltages compared with participation in sports that require more strength and speed and relatively less endurance
Examples of physiological changes that may be seen on ECGs of athletes include:
• Sinus bradycardia
• First degree A-V Block
• Incomplete right bundle branch block
• Early repolarisation
• Isolated QRS voltage criteria for left ventricular hypertrophy
While these changes may not be unusual in athletes, these findings should be interpreted in conjunction with their age, gender and levels of training, along with a full personal and family medical history to ensure the changes are consistent with their individual circumstances. Otherwise, further investigation may be warranted to exclude the possibility that these changes may be related to an underlying pathology.
Red flags
The 25-year Italian screening experience has demonstrated that 12-lead ECG has a substantial incremental value over and above history and physical examination for detecting asymptomatic athletes who have potentially lethal heart disorders.
Red flag changes which may be seen on an ECG, potentially identifying underlying pathology increasing the risk of sudden cardiac death include:
• T-wave inversion
• ST segment depression
• Pathological Q-waves
• Left atrial enlargement
• Left-axis deviation / left anterior hemiblock
• Right ventricular hypertrophy
• Ventricular pre-excitation
• Complete left or right bundle branch block
• Long or short QT interval
• Brugada-like early repolarisation
Unlike the relatively common ECG changes seen in athletes, the above ECG abnormalities are relatively uncommon (<5%) and cannot be attributed to training. Further diagnostic work-up is mandatory for those athletes who exhibit such ECG changes to confirm or exclude an underlying cardiovascular disease.
Who and how?
Bearing in mind the difficulties with screening young athletes, it is important to base decisions on who we screen and how best to do this on the best available evidence and guidance.
An excellent resource is the American College of Cardiology / American Heart Association 14-Element Cardiovascular Screening Checklist for Congenital and Genetic Heart Disease. (see box right) It is becoming increasingly common for local sports societies and associated medical bodies to have their own local guidelines in place.
It is vital not to underestimate the value of a good family history and family tree, including all first-degree relatives, nor the importance of a sound medical history including a systematic cardiovascular symptoms enquiry and full clinical examination.
There is no ideal single test that can detect all potential underlying triggers.
Symptoms with exercise, especially syncope or pre-syncope, should be taken seriously. In those where further screening using ECG is considered useful, remembering the normal physiological variants in athletes is vital in order to not increase false alarms for some athletes and cause a cascade of testing, which may be expensive and may cause unnecessary concern or limitation of activity.
The “Seattle Criteria4” have been developed to help distinguish normal ECG changes in athletes from abnormal and uncommon changes, and should be applied when the ECG is used as a screening tool. Using a refined Seattle criterion allows near perfect sensitivity and a low false positive rate (less than 5%).
Some patients may need further work-up by a cardiologist who is experienced in seeing athletes and in identifying the physiological changes in athletes’ hearts. Further investigations such as coronary artery imaging or stress echocardiography may be indicated.
Teaching resuscitation skills and how to use an automatic external defibrillator can save lives with early defibrillation and CPR to help maintain circulation.
Dr Jason Kaplan is cardiologist and clinical lead of the Cardiovascular Program, Macquarie University Health Sciences Centre. His clinical interests include sports cardiology, integrative and preventative cardiology and cardiac imaging.
References
1. Maron BJ, Levine BD, Washington RL, et al. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 2: Preparticipation Screening for Cardiovascular Disease in Competitive Athletes: A Scientific Statement From the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015;66:2356-61.
2. Steinvil et al . J Am Coll Cardiol. 2011 Mar 15;57(11):1291-6. Mandatory electrocardiographic screening of athletes to reduce their risk for sudden death proven fact or wishful thinking?
3. Corrado D et al. JAMA. 2006 Oct 4;296(13):1593-601. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program.
4. Drezner JA, Ackerman MJ, Anderson J, et al Electrocardiographic interpretation in athletes: the ‘Seattle Criteria’ Br J Sports Med 2013;47:122-124