The first national trial of home monitoring has shown the savings that could emerge from a large-scale rollout
The first national trial of home monitoring for chronically ill patients has demonstrated the savings that could emerge from a large-scale rollout
During the 12-month trial, undertaken by the CSIRO, telemonitoring almost halved MBS spending
and reduced PBS costs by one-quarter.
Hospital admissions were reduced by 53.2%, while the average length of stay in hospital dropped by 75.7%.
Based on the study, CSIRO estimates a potential $3 billion annual saving to the healthcare budget by providing telehealth services to the 500,000 Australian aged over 65 who would be good candidates for such a program.
“This is the first time we’ve done this in the Australian setting – a multi-site, multi-state study looking at the longitudinal difference for people with chronic illness,” Dr Rajiv Jayasena, who co-authored the report, told The Medical Republic.
“We have shown… there are economies of scale [with implementing telemonitoring], given that 70% of our healthcare spend is towards managing chronic diseases.”
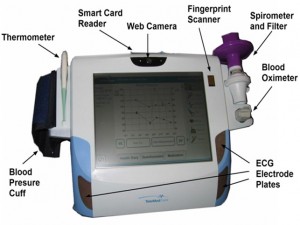
During the trial, patients with chronic illnesses measured clinically relevant vital signs every two days using a monitoring unit in their own home.
Patients suffered from chronic conditions such as cardiovascular disease, diabetes and asthma, and self-monitored parameters such as temperature, spirometry, oxygen saturation, blood pressure, glucose levels, and also performed ECGs.
The study involved 287 patients (including a control group of 173 patients) across the ACT, Townsville, Bacchus
Marsh and Melton in Victoria, Launceston in Tasmania and greater western Sydney.
During the trial, a nurse clinical-care coordinator regularly processed the data from around 25 to 30 patients from each trial site and coordinated a response, such as providing the patient with advice, involving the patient’s GP or recommending
the patient go to the emergency department.
“The key thing here is self management and picking up early deterioration and then intervening, so that patients won’t end up in hospital and costing the taxpayer a lot of money, as well as causing a lot of anxiety and depression when they end up in those situations,” Dr Jayasena said.
For example, a patient with chronic lung disease might keep a close eye on their oxygen saturation.
“Some of those events can be picked up by the device and the monitoring nurse because every day, or second day, data is looked at and you can see the gradual changes,” Dr Jayasena said.