Normalising sexual health conversations and boosting testing are key to tackling Australia’s rising STI rates, experts say.
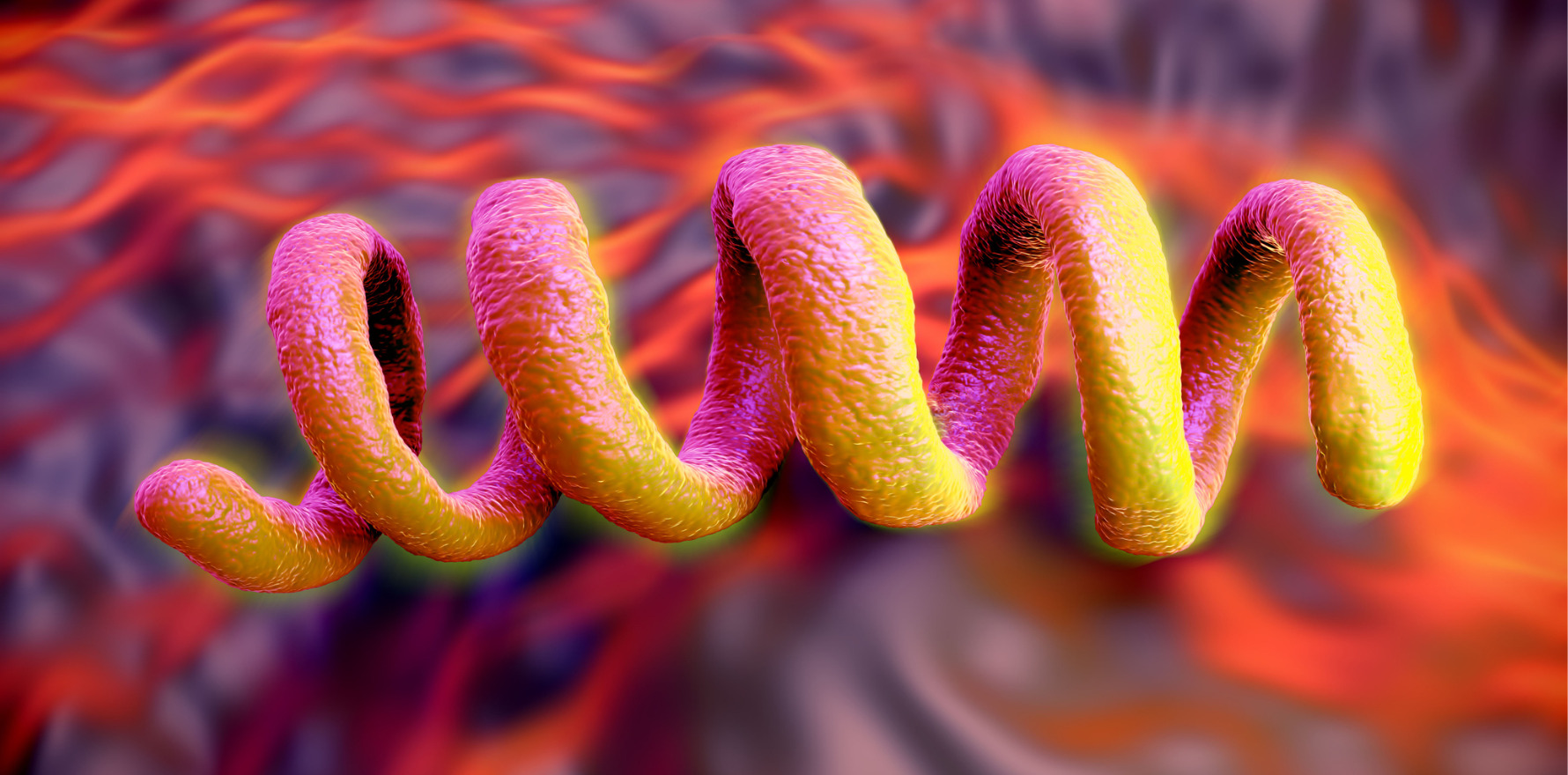
Rates of syphilis and gonorrhoea have more than doubled in Australia in the past decade and chlamydia numbers remain high, with experts warning that normalising conversations about sexual health is key to driving down STI rates.
The latest national surveillance data released by the Kirby Institute at the University of NSW shows that rates of congenital syphilis have also increased, but HIV notifications have dropped 27% in 10 years.
Lead author and epidemiologist at the Kirby Institute, Dr Skye McGregor, said rapid testing and early intervention were crucial to preventing the rise of sexually transmitted infections, and normalising discussions about sexual health was a key part of that.
“Having those discussions with new sexual partners, with regular sexual partners, having a discussion with your healthcare provider so these aren’t things that are kept in the shadows. We should be able to have conversations about our sexual health,” she said.
“The key thing is ensuring people get tested and treated early and the more we hide away from having those questions, the more we shy away from those difficult conversations, means that people are less likely to engage with their healthcare provider, less likely to have that discussion.”
Dr McGregor said a united approach was needed to help remove the discriminatory approach and stigmatising attitudes towards sexually transmitted infections.
There were more than 5800 diagnoses of syphilis last year – a doubling of cases in 10 years, Dr McGregor said. Eight out of 10 syphilis diagnoses were in men, but the number of cases in women has quadrupled in the last decade.
“This has significant implications, particularly in relation to congenital syphilis,” said Dr McGregor, who presented the data at the Australasian HIV&AIDS Conference in Adelaide.
“In this time period we’ve seen 103 congenital syphilis cases in Australia, which given we’re aiming for elimination of congenital syphilis, and this is entirely preventable, is a devastating outcome.
Related
“Around half of these cases are among Aboriginal and Torres Strait Islander infants, and over this period, tragically there were 34 infant deaths.”
Gonorrhoea numbers have also doubled in 10 years, with 44,210 gonorrhoea diagnoses in 2024. Seven out of 10 diagnoses are in men, Dr McGregor said.
“Rapid testing and treatment is really crucial to interrupt transmission. In the absence of other technologies like vaccines, prophylactic treatment, that is the key to getting rates down. It’s about early intervention,” she said.
Dr McGregor said some of the highest rates of chlamydia were among young heterosexual populations, and the recent Australian Sexual and Reproductive Health Survey found that only 16% of young people had ever been tested for an STI.
“Testing and early treatment is key to driving down those rates, but the rates of testing are so low among young people, we need to make sure the message is out there to get tested regularly.”
The researchers said diagnoses of chlamydia were relatively stable, but the infection remained the most common STI in Australia.
“Chlamydia continues to be the most commonly notified sexually transmissible infection in Australia, with over 100,000 notifications in 2024,” Dr McGregor said.
Some STI rates were higher among First Nations Australians, with chlamydia more than double, gonorrhoea almost four times higher and syphilis more than five times higher than in non-Indigenous people.
Robert Monaghan, a Bundjalung-Gumaynggir man and Manager of the Yandamanjang First Nations Health Research Program at the Kirby Institute, said the gaps were wider in regional and remote areas.
Mr Monaghan said it was “unacceptable” that in 2025, rates of STIs were two to five times higher among Aboriginal people in 2025.
“We need to be doing better and we need to be doing more,” he said.
“The community approach is essential. We need to co-design these programs with the community at the grassroots level so we can get a response that is community-led and have positive outcomes for our Aboriginal community.”
While HIV diagnoses have dropped 27% in the past decade, there has been a small increase in the past two years. That was most likely related to a decline in testing and low numbers of diagnoses during the covid pandemic, Dr McGregor said.
However, almost one third of HIV diagnoses were considered “late”, or in people who had been living with HIV for four or more years without knowing their HIV status, she said.
“These high proportions of late diagnoses are very concerning. We need to ensure HIV testing is accessible, including self-testing, to ensure timely diagnosis and engagement in appropriate care for people with HIV,” she said.
Dash Heath-Paynter, CEO of Health Equity Matters, said the right tests needed to be available in the right places to ensure people test more frequently.
“We need more targeted testing and investment to ensure all gay and bisexual men, and men who have sex with men, can test frequently enough,” he said.
Injection drug use accounted for 19 HIV notifications in 2024, which Dr McGregor said reflected Australia’s sustained and successful response to HIV among people who inject drugs.
Dr McGregor said there had been a halving in the number of HIV notifications in the last 10 years among people born overseas, but little change in numbers among people born overseas.
“We need to really focus on the groups that aren’t experiencing declines equally, and understand where the places of greatest need are, whether it’s early engagement in testing and care, or access to treatment and rapid engagement to ensure people have the healthiest outcomes possible,” she said.