The new drug led to significantly improved survival in patients with hard-to-treat cancer, prompting a fast-track approval process in the US.
The FDA have moved to expedite the approval of a new therapy for forms of ovarian cancer that currently lack effective treatment options.
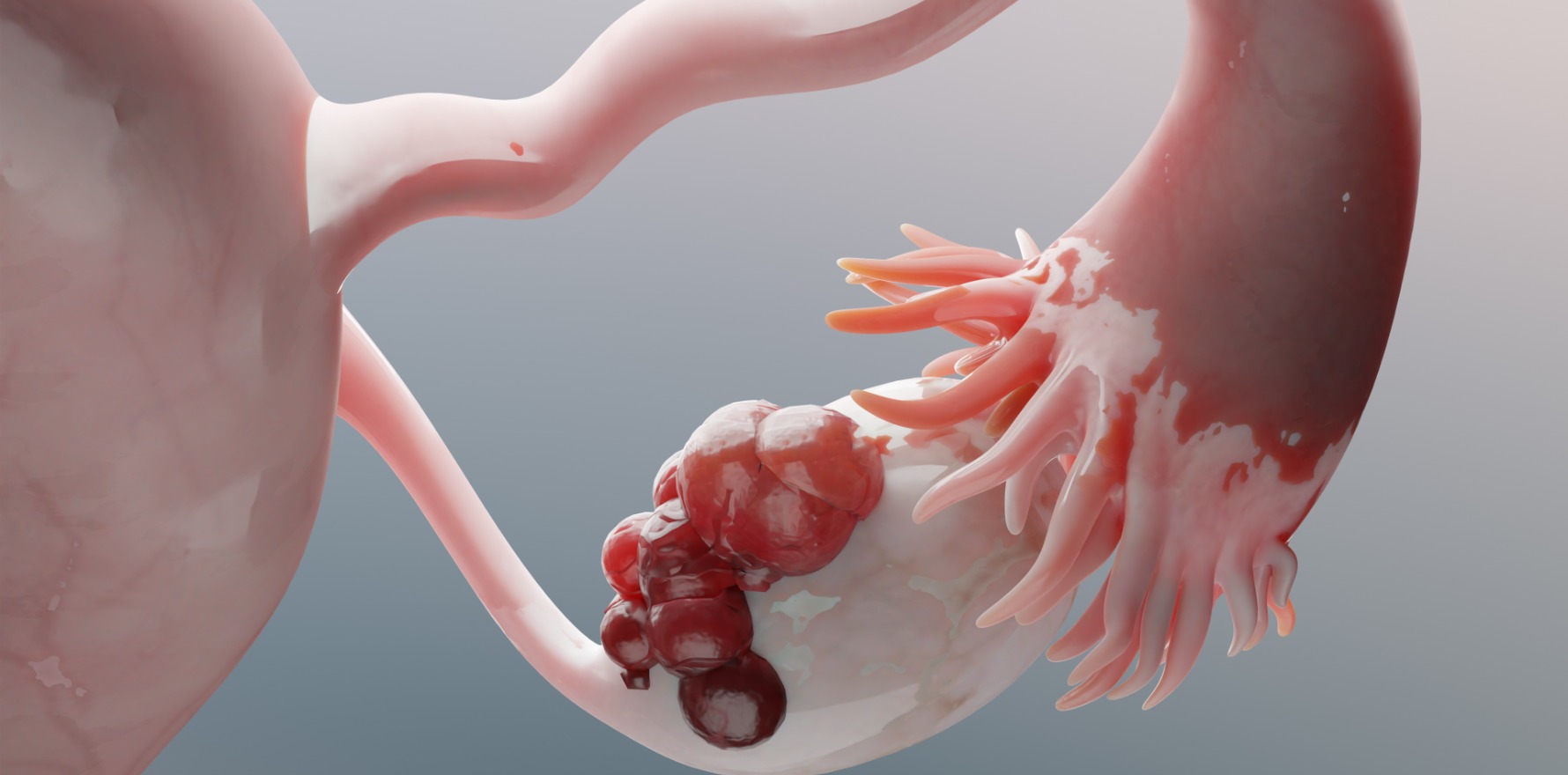
Patients with newly diagnosed stage IIIb-IV ovarian cancer are typically treated with debulking surgery and combination chemotherapy, although this approach is associated with high relapse and low survival rates. PARP inhibitors and checkpoint inhibitor therapy have also been trialled in these patients with little success.
But a recent clinical trial has investigated the potential benefits of an immunotherapy-based approach involving gemogenovatucel-T. The latest findings from the trial have been published in JCO Precision Oncology and suggest the drug improves survival relative to placebo.
“Gemogenovatucel-T is a DNA-engineered triple function immunotherapy using autologous tumour cells as a source of the full matrix of a patient’s tumour-related clonal signals,” the researchers wrote.
“[The] gemogenovatucel-T product clonal tumour mutation burden (cTMB) signal comprises the same clonal DNA mutations as the harvested autologous tumour used to construct gemogenovatucel-T.”
Researchers used data from the VITAL trial, where 91 patients with frontline stage IIIb-IV ovarian cancer in clinical complete response following debulking surgery and adjuvant or neoadjuvant chemotherapy were randomised to receive either gemogenovatucel-T (n = 47) or placebo (n = 44) as maintenance therapy. The final analyses included 11 patients in the gemogenovatucel-T group and 12 patients in the placebo group.
Patients with high cTMB and HRP-type tumours who received gemogenovatucel-T were 77% more likely to survive compared to patients who received placebo.
The effect of gemogenovatucel-T on overall survival remained after seven years, with 45% of patients who received active treatment alive at this time point compared to 8% of patients in the placebo group. Analyses estimated that the median overall survival was 68 months in patients treated with gemogenovatucel-T and 19 months for patients who received placebo.
Treatment-related adverse events occurred at a similar rate between the two groups of patients, with injection site reactions the most commonly occurring event for both gemogenovatucel-T (36%) and placebo (25%). Other reported grade 1-3 treatment-related adverse events included abdominal pain, diarrhoea, nausea, fatigue and pain. There were no grade 4 or 5 treatment-related events in either group.
“Treatment with gemogenovatucel-T promotes (1) patient tumour-specific clonal neoantigen presentation, (2) dendritic cell activation (via plasmid expression of granulocyte-macrophage-colony-simulating factor) and (3) tolerance escape (via plasmid generated interference of transforming growth factor-β1, transforming growth factor-β2 expression consequent to reduction of expression of the furin cleavage enzyme),” wrote the researchers.
The current analyses were limited by the small sample size. But the US Food and Drug Administration were suitably convinced by the findings of the VITAL trial to grant gemogenovatucel-T Fast Track (Regenerative Medicine Advanced Therapy), progressing with the development, review and possible approval of gemogenovatucel-T for use in the United States.