After over a decade of stability, the proportion of GP fees subsidised by Medicare has tumbled.
Following 15 years of little to no change, the proportion of GP fees covered by the MBS has dropped six percentage points over just 18 months and is now sitting at one of the lowest rates on record.
In other words, the amount that people are paying out of pocket is increasing.
Between 2005 and 2020, Medicare picked up about 90% of the bill for GP-related attendances.
It reached a high of 95% in April 2020, remained high for the bulk of covid vaccinations in 2021 and regressed back to the mean of around 91% in January 2022.
New data from the Australian Institute of Health and Welfare shows that the July 2023 MBS coverage rate of 84.83% is a low that has only been eclipsed four times before.
Those four times were January, February, March and June 2023.
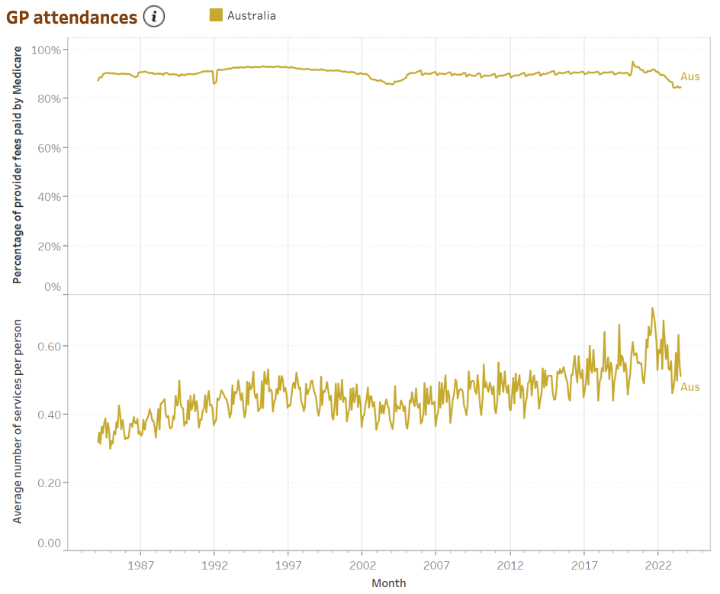
There has also been a trend toward more services per person over time.
“This data shows quite clearly the cost of healthcare is significantly outpacing the Medicare system, causing even higher out-of-pocket costs for Australian patients,” AMA president Professor Steve Robson said.
While the tripled bulk billing incentive and second round of MBS indexation were welcome inclusions in the May budget, Professor Robson said Medicare reform was “still a work in progress”.
“The chronic underfunding of Medicare has had a direct impact on the hip pocket of Australians, which is being acutely felt now as we are in the middle of a cost-of-living crisis,” he said.
Before the pandemic, the only times that the proportion of GP fees paid by Medicare had dropped even close to 85% was late 2003 through to early 2004 and for a few months between December 1991 and April 1992.
General practice isn’t the only MBS area to receive decreasing proportions of Medicare money. Specialist attendances, surgical operations, obstetrics and allied health services have also trended downward with time, even as Australians access more services per person.
The only exceptions to this rule are pathology, which continues to receive around 94% of provider fees from Medicare – which it has done quite steadily since about 1995 – and diagnostic imaging, which has long sat at a proportion of about 85% Medicare funded.