A radical proposed shakeup would give GPs more low-intensity mental health services and relieve the 'choke' in the system.
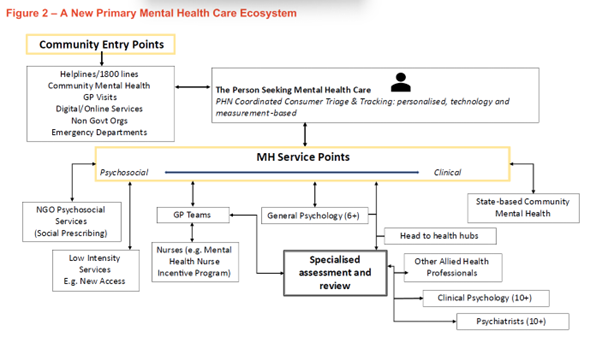
Introducing a triage and tracking system run by PHNs and populating lower tiers of care with more “low-intensity services” are among new proposed solutions to Australia’s struggling primary mental health services.
Dr Sebastian Rosenberg and Professor Ian Hickie, from the University of Sydney’s Brain and Mind Centre, today published a discussion paper which posited a three-step rejigging of the way patients access mental health care.
At the heart of the plan are two new central features:
- a coordinated triage and tracking system run by the PHNs, “providing personalised measurement using technology to help people find the right clinical or psychosocial service, assess the impact of those various interventions and determine next steps”; and,
- a specialised initial assessment and review function “aiming to better coordinate the professional response to a person’s mental health and psychosocial needs”.
Pulling it all together, the authors say, is dependent on the development of a national digital infrastructure “to underpin rapid assessment, smart triage to appropriate levels of clinical and psychosocial care and ongoing coordination of care”.
The aim is to shift the focus of care delivery away from general practice and emergency departments.
“These shifts will permit both those two key service elements to focus on their core functions,” wrote Dr Rosenberg and Professor Hickie.
“For general practice, that means a key role in the coordination and delivery of more complex care to those with comorbid physical health difficulties, and for EDs, the urgent assessment and delivery of responding to life-threatening situations.”
The PHNs, they wrote, “using personalised approaches and technology, would be responsible for establishing and directing individual primary mental health care journeys and monitoring the impact of the care provided”.
Dr Rosenberg told TMR that “some of the uncertainties and unspoken ways of doing things” in the mental health system needed to be replaced by “a more explicit design of service response”.
“At the moment, you have psychiatry and clinical psychology operating exactly the same way as other specialist services, in isolation from each other, on a fee-for-service basis with little or no responsibility for this kind of assessment and review,” he said.
“It’s a new function that would need to be instituted, to make it more likely that a person gets to the right level of care, as opposed to being lost in a spiral.”
In the discussion paper, Dr Rosenberg and Professor Hickie wrote that “simply training more health professionals to work in this disorganised way will not be enough”.
“Australia’s mental health care and psychosocial support systems need to be radically reorganised. We need to help people get on the right clinical or psychosocial tracks as quickly and as easily as possible.”
The concept is that putting patients at the right level of care from the very first opportunity will free up psychology and psychiatry hours for those patients needing high-intensity care.
The addition of mental health nurses, social prescribing, Head to Health hubs and other low-intensity services will also lift some of the burden from GPs, they wrote.
“Our proposal would actually reinforce the role of general practice in coordinating the delivery of more complex care for those with comorbid, physical health, but they would not be one of the ‘front doors’, because it would be populated with a range of other services,” Dr Rosenberg told TMR.
“Clearly, if we’ve got our resources better organised, and we’re better able to respond more accurately to the different needs people have, then we’re likely to be able to free up parts of the system, which are now choked,” Dr Rosenberg said.
“We have a situation now where about 70% of people in the system are repeat customers. They have not received the care they need. They are stuck in the system and not recovering.
“But simply putting more funding into that existing system will not alleviate that choke.
“We need to create a more sensitive assessment and titration of our precious mental health workforce, to better meet the needs of people.
“That’s why the specialised assessment is really critical for people so that we deploy those with most expertise, shall we say, in mental health, particularly psychiatry and clinical psychology to help the system with that process of titration and getting people to the right level of care from the start.”





