And GPs, as usual, are picking up the slack.
New research confirms that, similarly to many other healthcare services, “severe inadequacies” plague regional and remote mental health care, says the National Rural Health Alliance.
But it’s GPs who are at the “coalface” of the mental health crisis, especially for rural and remote communities, according to RACGP president Nicole Higgins.
The National Study of Mental Health and Wellbeing in 2022 showed that almost half of Australians are subject to a mental health condition in their lifetime.
It’s therefore unsurprising that for GPs almost 40% of consultations involve mental health, the most recent RACGP Health of the Nation survey suggested.
In fact, according to the survey, patients are more likely to see a GP for mental health concerns than any other health professional.
GPs are generally the first point of contact for mental health care in Australia, Dr Higgins said in a statement.
“GPs are the cost-efficient engine house of the healthcare system – we keep people healthy and out of hospital. And we do a lot when it comes to mental health care, which many people don’t realise,” she said.
“Across Australia every day, GPs are at the coalface delivering care and supporting patients as well as their families through their mental health journey. We have a wealth of knowledge and experience to contribute to help Australia address its mental health crisis.”
This is particularly evident in regional and remote communities, where GPs provide almost all the mental health care, according to the college’s survey.
Dr Higgins drove home the “urgent” need for more Medicare funding for the longer consultations necessary for these complex disorders to ensure that “no patient misses out on the care they need”.
“Mental health consultations cannot be rushed, these are complex and often very sensitive issues,” she said.
“Longer consultations need to be affordable for anyone who needs them, no matter where they live or how much they earn.”
Also championing the need for investment to address access in a recent media release, the NRHA called for “systemic mental health reform” and “increased investment” to address the “alarming” disparities shown in Mapping Mental Health Care research project’s recently released data.
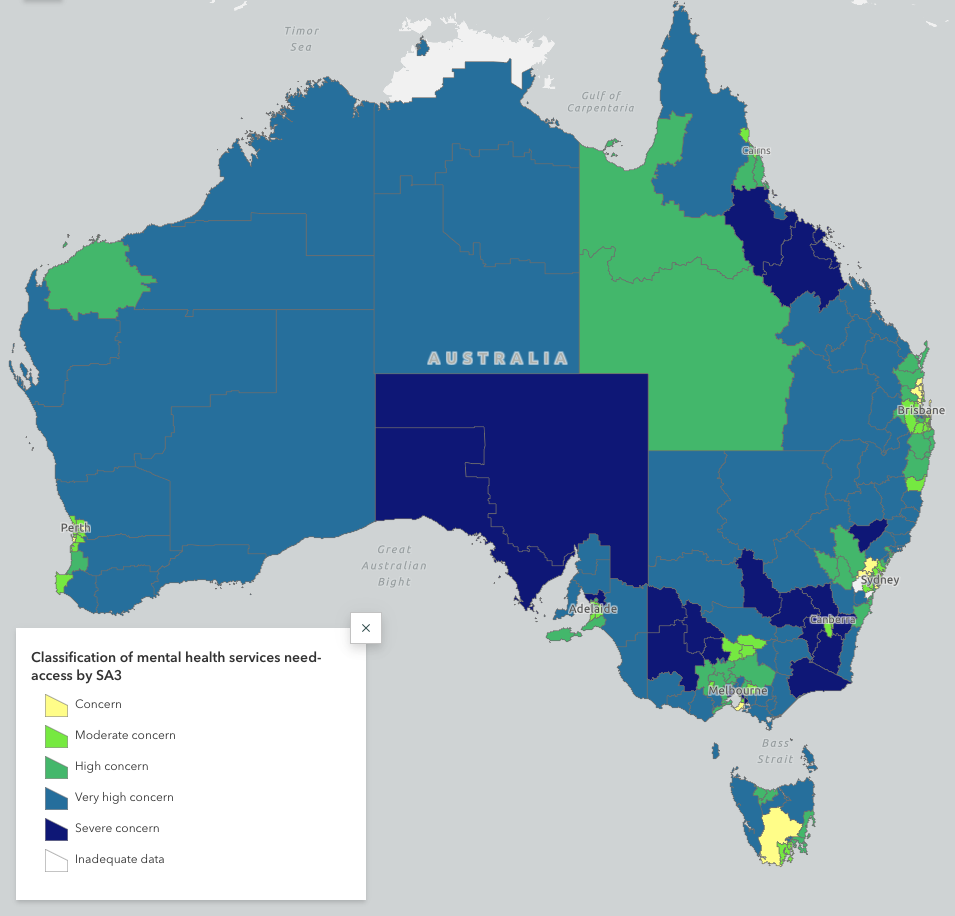
The project, which was a joint venture by Mental Health Australia and the National Centre for Social and Economic Modelling at the University of Canberra, looked at where Medicare-based mental health services were falling short of demand.
The researchers ranked areas as of “concern” – lower need and higher service access – to “severe concern” at the opposite end of the spectrum. Most of the country fell into the very high or severe concern categories.
Susi Tegen, chief executive of NRHA, called for “more commitment” from all levels of government to “engage with stakeholders to relieve rural communities of the barriers to accessing mental health services”.
“The latest data is a wake-up call on World Mental Health Day, to take urgent action to provide care every day for people living outside cities. We have a social contract to do so,” said Ms Tegen.
“We know mental illness in rural and remote Australia appears more prevalent than in major cities and tragically, rates of self-harm and suicide increase with remoteness. Yet, these communities are the most underserved compared to major cities.
“We need to address the unique problems faced by rural, regional and remote communities and attend to them with innovative, place-based, flexible models of mental health care and funding.”




