Instead of introducing a new class of providers, the AMA argues that the government should focus on making training accessible for the current workforce.
The AMA is warning against allowing endorsed midwives access to MBS rebates for inserting long-acting reversible contraceptive (LARC) devices, calling a lack of existing safety data “concerning”.
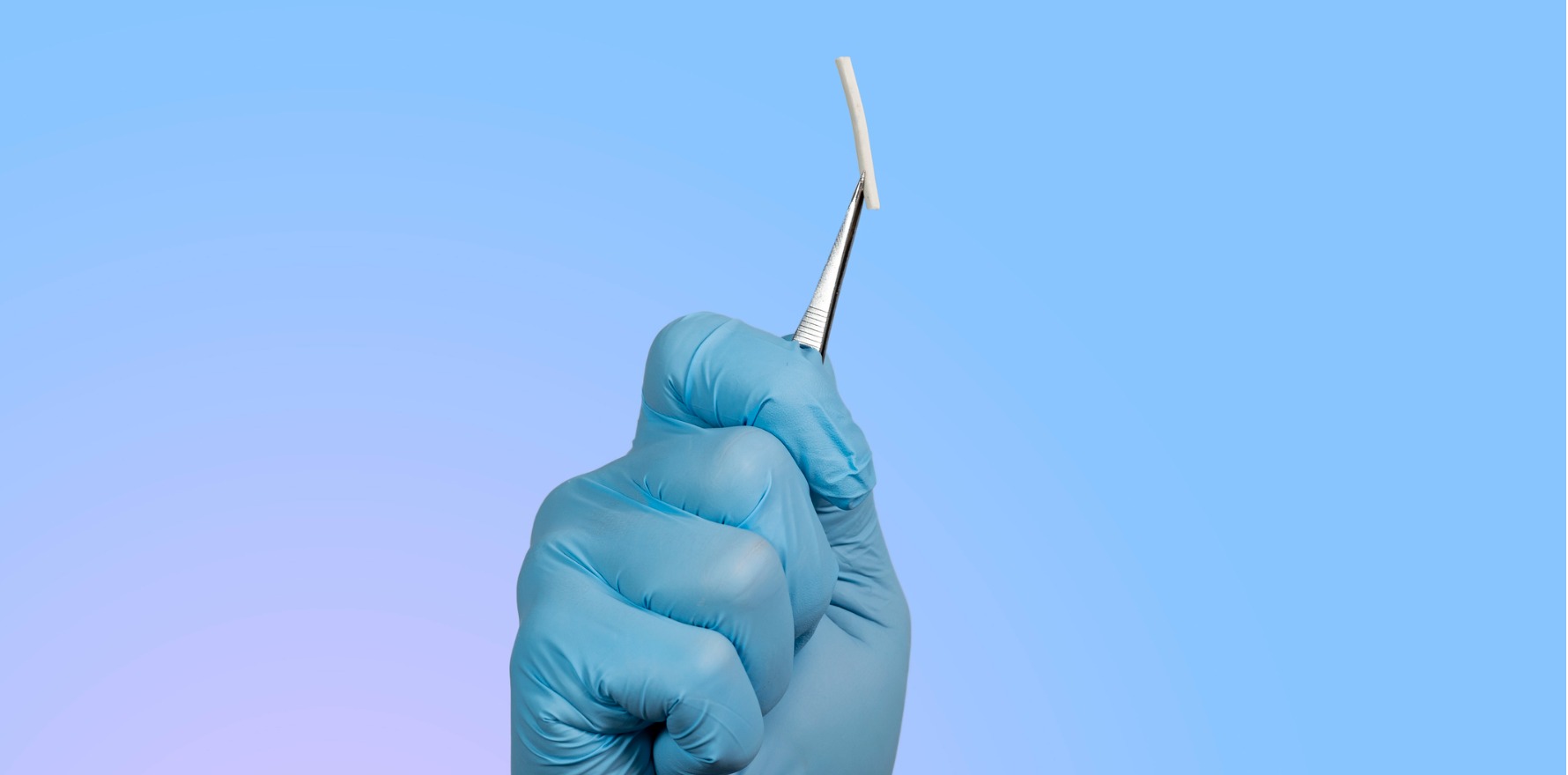
It joins the RACGP in pushing back against an MBS Review Advisory Committee draft recommendation to expand MBS access for hormonal implant and IUD insertion and removal to endorsed midwives, a subgroup of midwives who have typically completed additional study and are qualified to prescribe scheduled medicines.
There are currently just 1507 endorsed midwives in Australia. Of these, 1506 are endorsed for scheduled medicines and one is endorsed as a midwife practitioner.
The MBS access would only extend to LARC insertion or removal for the purposes of contraceptive care, and would not include complex removal processes involving anaesthesia.
The AMA appears to be concerned with the prospect of endorsed midwives inserting IUDs specifically.
“[Endorsed midwives] and other midwifery or nursing professionals, though highly skilled, are not trained in intrauterine instrumentation (such as cervical dilation, paracervical block, or managing cervical shock/fainting) and do not have the scope of practice or spectrum of skills required to perform these procedures autonomously or without medical oversight,” the association’s submission read.
On the hormonal implant, however, the AMA took a slightly different view.
“If any consideration is given to contraceptive implant insertion by [endorsed midwives], it should only occur where the midwife is also credentialled as a nurse practitioner, with dedicated training and clinical governance comparable to MS-2 Step arrangements, and with clear escalation pathways to GP/gynaecology care,” it said.
As of October 2025, nurse practitioners have access to MBS items for LARC insertion and removal, making this point somewhat moot.
The AMA also took issue with a lack of existing safety data.
“It is concerning the department intends to proceed with substantial policy changes when it is unable to provide robust data on the current extent of LARC services delivered by [endorsed midwives],” the AMA said.
“Evidence-based reform should be underpinned by a clear understanding of existing service delivery patterns, including the number of [endorsed midwives] performing LARC procedures, the settings in which these occur, and the outcomes for patients.
Related
“The absence of such data introduces unnecessary risk and uncertainty into the policy process.”
Only once there is a comprehensive understanding of the current and potential contribution of endorsed midwives, the AMA said, should the question of expanding MBS items revisited.
Despite being opposed to endorsed midwife involvement, the AMA said it supports the overarching aim of improving access to LARC services in primary care.
To this end, the association said the most effective route to improved patient access to LARCs is through addressing persistent GP training bottlenecks and service provision barriers, rather than adding provider groups.
On its own, contraceptive implant training costs around $240 minimum and IUD insertion training costs between $1500 and $1995.
The government now funds scholarships to cover training costs and subsidies for practitioners who are travelling in from rural areas to attend in-person workshops.
In February, it also announced a $25.1 million investment to establish eight LARC centres of training excellence to improve availability of training.
“Internal consultations with AMA members consistently highlight the principal barrier to expanding LARC access is not a shortage of willing providers, but rather a significant bottleneck in training opportunities for GPs,” the AMA said.
“Many GPs are eager to offer LARC services but face protracted delays – sometimes several years – before they can access accredited training.
“The recent government commitment of $25.1 million to establish Centres of Training Excellence is a welcome development, but its success will depend on transparent implementation and a clear focus on reducing GP wait times.”