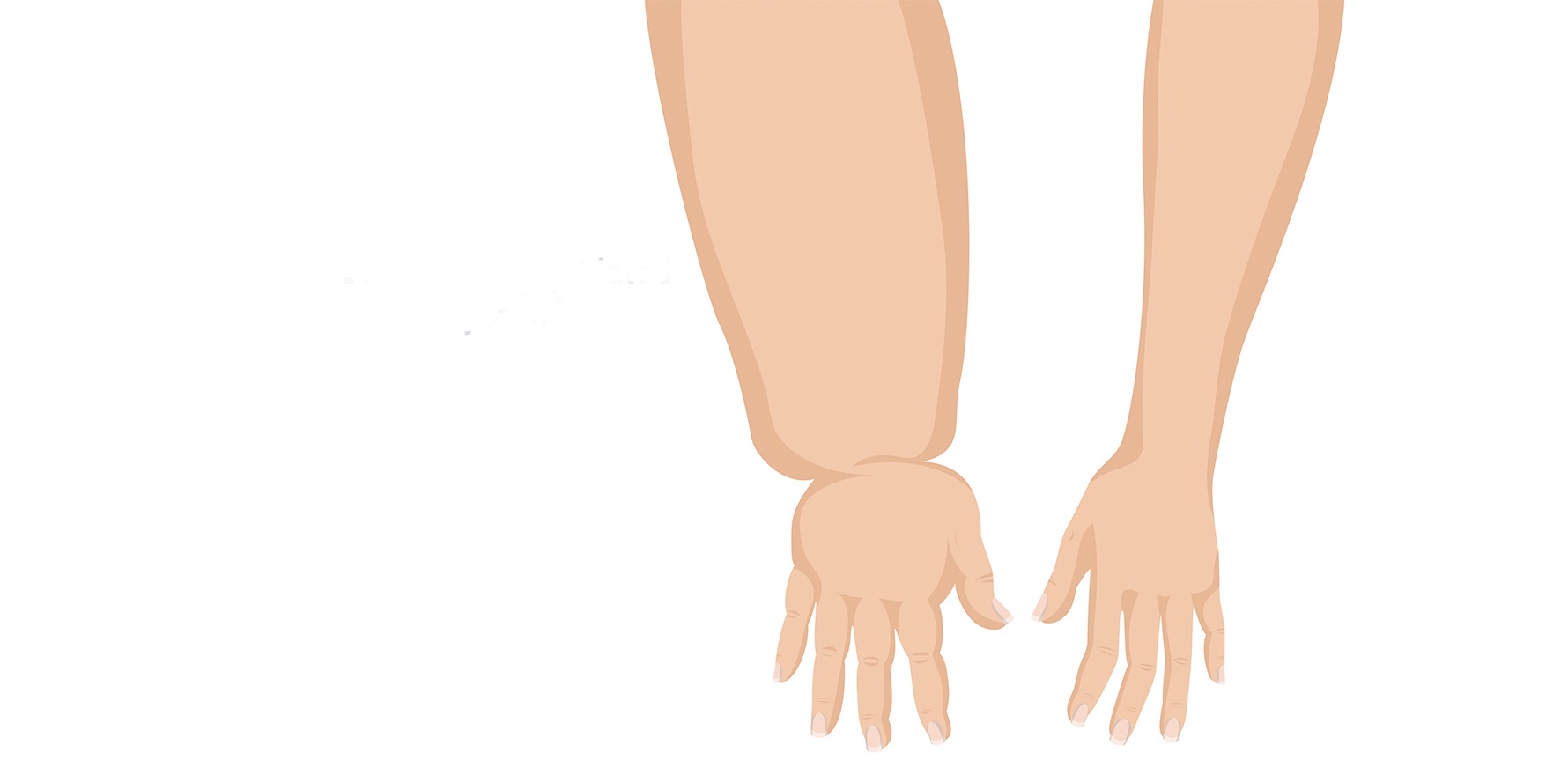
Lymphoedema can strike decades after treatment, and while it’s not preventable, catch the signs early enough and you can stop it becoming chronic.
It’s estimated that around one in five people treated for breast cancer will develop arm lymphoedema.
About 50% of cases of breast cancer-related arm lymphoedema occur in the 12-30 months post-surgery, others many years later. Once it becomes chronic, it cannot be eradicated.
An international study led by the Multinational Association of Supportive Care in Cancer (MASCC) has published guidelines on who is most at risk, prospective surveillance and the use of interventions, including compression sleeves.
“The impact of lymphoedema on individuals and the healthcare system is profound,” says lymphoedema researcher, Professor Sandi Hayes from the Menzies Health Institute Queensland.
“Lymphoedema adversely affects all aspects of life – the ability to work and function, psychosocial wellbeing, relationships.”
She told TMR the MASCC guidelines “rightly highlight” the unmet need for breast cancer survivors.
“Educating patients about the signs and symptoms of [arm lymphoedema] are highly important to ensure patients know when to seek early medical attention,” the authors said.
However, patients need to be given evidence-based advice, they said.
For instance, patients have been told to avoid having blood pressure taken on the at-risk arm and to wear a compression sleeve when flying, neither of which were found to be correlated with developing arm lymphoedema in large studies.
“Patients may have a false sense of security after adhering to these lifestyle modifications if the recommendations are not supported by evidence,” the authors said.
The effectiveness of compression sleeves is an area that needs more research, said Professor Hayes.
“Wearing compression sleeves comes with its own issues that women don’t like. It’s hot, it’s uncomfortable, it’s restrictive. It tells me and it tells the world ‘I’m a breast cancer patient’. From a clinical-based perspective, clinicians will tell you that actually a poorly fitted garment will be worse than no garment at all.”
In addition, compression garments typically cost from $100-$400 but can cost even more. Two are needed to rotate washing and wearing, and they last about six months, she noted.
Professor Hayes told TMR there was strong evidence to support some risk factors – the more lymph nodes removed, the higher the risk; moderate level evidence for others – chemotherapy, insufficient physical activity; and low, confusing or no evidence for others, such as increased age.
And the evidence for various risk factors and interventions has changed over time, Professor Hayes explained.
“For example, in the past chemotherapy was not considered to influence risk whereas now it does; radiation was considered to be strongly associated with lymphoedema, whereas that relationship remains present but has become weaker over time (likely to do with more targeted radiation techniques) and is influenced by whether the axilla is involved or not.”
“Then you have a risk factor such as higher body mass index. This one may be dependent on how [arm lymphoedema] is measured. To date, we have no evidence to support weight loss reducing risk or improving management,” she said.
“People who have had lymphoedema in the past have had comments given to them like, ‘If you lost weight, you would have better control of your lymphoedema’. Or, ‘If you weren’t fat, you wouldn’t have got lymphoedema’. That’s actually not necessarily the case.”
Dr Nina Stewart, a radiation oncologist at GenesisCare in Western Australia, said she has seen rates decrease over the last decade due to awareness, early intervention and management. And while it was not yet commonplace, more surgeons were becoming skilled in reverse mapping and prophylactic reconstruction.
“There is significant emphasis on early detection and prophylactic compression. I would say almost all of my patients have been reviewed by a lymphoedema therapist prior to seeing me, with bioimpedance spectroscopy and compression sleeve in the majority, and otherwise a referral has almost always been done,” she said.
But Professor Hayes said that outside the major cities, access to specialist care in Australia is limited, making patient and practitioner knowledge about lymphoedema and its signs and risk factors particularly important.
“This will have a flow on effect to patients by helping them to become aware of early signs and symptoms, and to participate in healthy lifestyle practices that will benefit their lymphoedema risk but also their risk of other common cancer treatment-related side effects (e.g., fatigue).
“Further, in the instance that lymphoedema associated symptoms presents, better educated members of the healthcare system would ensure that when a patient presents with these concerns to their GPs or oncology team, their symptoms will be acknowledged and dealt with, rather than dismissed as normal physiological responses to the treatment that will subside with time.”
The MASCC consensus involved 55 experts and made 23 recommendations, including the following:
- The five biggest risk factors for arm lymphoedema are axillary lymph node dissection, post-operative radiotherapy, relative within-arm volume increase one month after surgery – all of high importance – followed by greater number of lymph nodes dissected and high BMI. Evidence suggests timing and type of chemotherapy should not be “major determining factors” in deciding whether to offer prophylactic options.
- Prospective surveillance programs should be started three months after surgery, with patients monitored every three to four months in the first year, then six to 12 months for at least two years.
- When lymphoedema is detected, compression sleeves are recommended as an early option for at least four to six weeks, with more intensive treatment, such as complete decongestive therapy, for more advanced cases.
- Compression sleeves are also recommended as an option for at-risk patients, from the first day after surgery to three months after adjuvant therapy ends, to be worn for at least eight hours a day where possible. However, patients should be advised that the value of compression sleeves beyond a year is uncertain.
- Axillary lymph node dissection should not be routine for T1–2, node negative breast cancer patients with 1–2 positive sentinel lymph nodes who have breast conservation therapy. For those who have a mastectomy, consider axillary radiation instead. Axillary lymph node dissection is recommended for those with more than two positive sentinel lymph nodes. With axillary radiation, moderate hypofractionation is recommended, with consideration of cardiac risk factors and tumour site. The possible correlation between axillary radiation and second primary cancers is unclear.
- Prophylactic lymphatic reconstruction is recommended as an option for patients who need extensive axillary lymph node dissection.
- Axillary reverse mapping, a technique used during surgery to identify disruption to the drainage channels, is recommended as an option for some patients who have had axillary lymph node dissection, but not for those at high risk of axillary recurrence.
The latter two options – both “sophisticated surgical techniques that require specialised training to perform” – are not widely taken up at present, and given the availability of cheaper methods (like sleeves) might not end up being cost effective, though the data on that is not yet in.
The MASCC recommendations were based on randomised controlled trials and systematic reviews and complement the 2022 consensus on diet, skin care and exercise.
The authors noted that thresholds for treatment were recommended based on studies from North America and Europe and there could be variations in different local populations.
“Practitioners should remain flexible and carefully discuss with patients the pros and cons of initiating interventions when thresholds are met, taking into account whether patient has any symptoms and risk factors of [breast cancer related arm lymphoedema,” the authors noted.