Cataracts, the leading cause of blindness worldwide, can be treated safely, precisely and predictably
Cataracts cause 40% of cases of visual impairment in Australians aged 55 and over, and there are currently over two million Australians in this age bracket who suffer from untreated cataract, most of whom live in remote and regional Australia. Globally, cataract is the leading cause of blindness.
There are several different types of cataracts, including nuclear, cortical, sub-capsular and mixed cataracts.
Each type affects a particular anatomical location within the crystalline lens and has specific pathological processes and risk factors for their development.
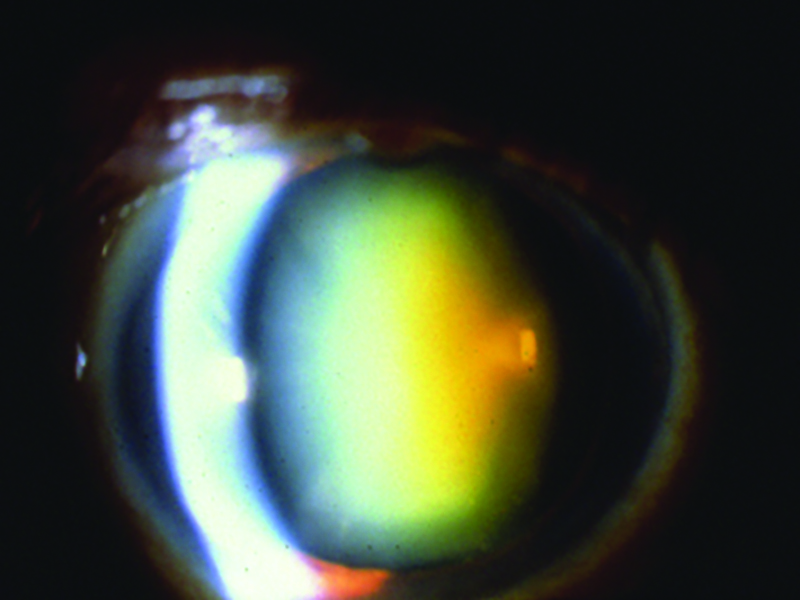
In Australian patients, nuclear cataract is the most common type, and consists of a central opacification or yellow discoloration that interferes with visual function. Nuclear cataracts tend to progress slowly and affect distance vision more than near vision. Nuclear cataracts may induce myopia or a reduction in pre-existing hyperopia.
Increasing frequency of changes in the prescription of spectacles may be an early sign of cataract formation.
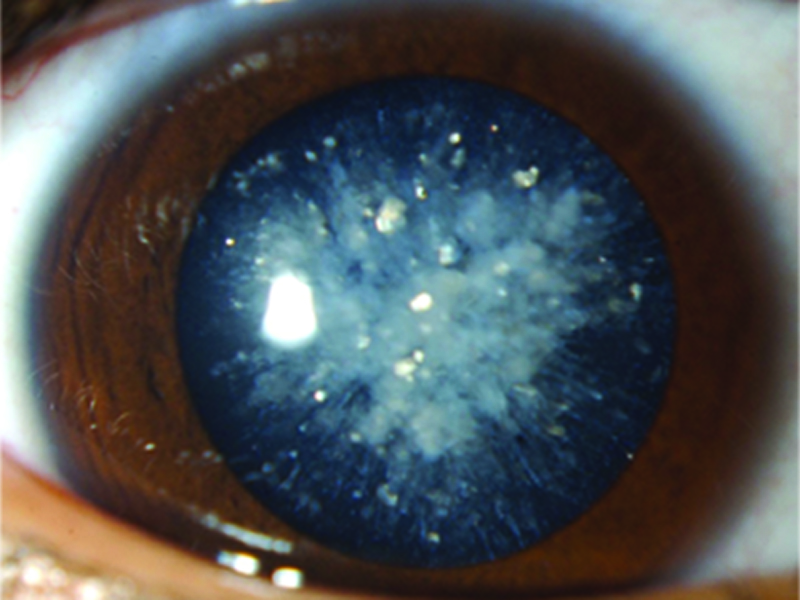
Cortical cataracts are spoke-like in appearance. Patients with this type of cataract commonly complain of glare, especially while driving at night. As a result, elderly patients often stop driving in conditions of low light and low contrast, but cannot always directly ascribe this to poorer quality of vision.
Posterior subcapsular cataracts are found more often in younger patients than either nuclear or cortical cataracts. Patients often have glare and poor vision in bright light, and near vision is typically more affected than distance. This type of cataract is more common in diabetic patients or those who have used systemic or topical corticosteroids. Posterior subcapsular cataracts progress more rapidly than other types, and can result in significant impairment in vision in only a few months.
Advancing age is by far the most important risk factor for cataract development, such that most individuals have some degree of cataract by their mid-60s. Other risk factors include diabetes mellitus; long-term use of topical, systemic, intravitreal, inhaled or oral corticosteroids; prior intraocular surgery; or significant ocular trauma.
The impact of a cataract on visual function can be subjectively assessed by self-reported functional status or difficulty with vision. However, patients may adapt to their visual impairment, and may fail to notice the functional decline that accompanies the insidious progression of a typical cataract. It is equally important to note that the impact of cataract is not limited to a reduction of distance visual acuity, as measured on a Snellen chart, this being a very narrow measure of a person’s visual function.
Other important facets of visual function including near vision, vision in dim lighting or situations of low contrast (e.g. dawn or dusk), glare, impaired colour vision or peripheral vision, and depth perception, can all be adversely affected by a significant cataract.
Loss of vision in the elderly can, in addition, be associated with a decline in physical and mental function, as well as a loss of independence in activities of daily living. Visual impairment caused by cataract is an important risk factor for falls and hip fractures, and a significant reduction in the rate of falls and fractures after cataract surgery has been demonstrated in randomised controlled trials. Drivers with visually significant cataracts are also 2.5 times more likely to have an at-fault motor vehicle crash, compared with drivers without cataracts.
In short, it is well established that physical function, mental health, emotional wellbeing, safety, and overall quality of life can be enhanced when visual function is restored by cataract extraction.
PREVENTION
Preventive measures that impart even a modest decrease in the risk of cataract could have a large public health impact, given that millions of people are affected by cataracts in Australia, with numbers set to grow as our population ages.
Several studies show a link between smoking and nuclear cataract, demonstrating a dose-response effect. Smoking is also associated with an increased risk for posterior subcapsular and, to a lesser degree, cortical cataract.
Cumulative lifetime exposure to ultraviolet-B radiation has also been associated with cataract development. Therefore, brimmed hats and ultraviolet-B blocking sunglasses are reasonable precautions to recommend to all people.
There is some evidence that long-term multivitamins may decrease the risk of nuclear cataract but not enough to guide recommendations for their use.
However, little evidence exists that long-term high-dose antioxidant supplements (Beta-carotene, Vitamin E and C, lutein/zeaxanthin) or Omega-3 long-chain fatty acids, such as those in fish oil, decrease the progression of cataract.
There is also some evidence that a diet rich in fruits, vegetables, and wholegrains may reduce the progression of cataract, with vegetarian and pescatarian diets also conferring a protective effect compared with diets containing red meat.
HISTORICAL PERSPECTIVES
The history of cataract surgery is interesting and worth visiting. It is one of the oldest surgical procedures known, first documented in the 5th century BC. In ancient times, cataracts were treated with a technique called “couching”. The eye would be struck with a blunt object with sufficient force to cause the zonules to break, so that the lens would dislocate into the vitreous cavity, restoring limited but completely unfocused vision. Centuries later, the technique was modified so that a sharp fine instrument was inserted into the eye to cause the dislocation.
The first reported surgical removal of a cataract from the eye was in Paris in 1748, when the advent of topical anaesthesia made the procedure more practical and palatable. Using the early techniques, the entire opaque lens was removed in one piece using an incision that went halfway around the circumference of the cornea. It was critical that the lens remained intact during removal, so surgery was restricted to so-called ripe or “mature” cataracts.
This limited the surgery to only the most advanced cataracts. Since fine sutures did not exist at that time, patients were kept immobilised with sandbags around their head while the wound healed, with many eyes lost to infection. The early literature routinely documented the mortality rate from cataract surgery, an almost unheard of phenomenon in the current day, secondary to pulmonary emboli.
The most significant change in the modern era was the introduction of phacoemulsification surgery in 1967 by Dr Charles Kelman. In this technique, ultrasonography is used to break the lens into minute fragments that can be aspirated (termed phacoemulsification). A combined ultrasonographic irrigation and aspiration hand piece allows the removal of any lens (hard or soft) through a small incision. This revolutionised cataract surgery, with modern day corneal wounds routinely less than 3mm in size.
Originally, no intraocular lens implants were used following cataract surgery, and patients had to rely on “Coke bottle”- thick hyperopic glasses. At a later date, thanks to the pioneering work of Howard Ridley, a British ophthalmologist, intraocular lenses were developed. Ridley recognised that the penetration of shattered fragments from airplane windshields into the eyes of World War II fighter pilots did not always lead to damage, and went on to create the first artificial lens from the same material.
The evolution of smaller surgical incisions was matched by the development of new lens implants that could be folded to allow the lens to be inserted through a tiny wound. At present, commercially available lenses can be inserted through wounds as small as 2mm.
The predominant method of cataract surgery used in the developed world today is suture less small-incision phacoemulsification with foldable intraocular lens (IOL) implantation. Cataract surgery is one of the commonest and most effective procedures in modern medicine, and in 2013–14, approximately 160,500 cataract surgical procedures were performed in Australia.
The primary indication for cataract surgery in the developed world is visual function that no longer meets the patient’s needs, and for which cataract surgery provides a reasonable likelihood of improved vision. Other indications for cataract removal include clinically significant anisometropia (a large difference in the focusing power of the two eyes), or presence of a cataract that interferes with optimal diagnosis or management of posterior segment conditions such as diabetic retinopathy. A cataract that causes inflammation or secondary glaucoma should also be removed.
Pre-operative medical evaluation
The pre-operative evaluation of the cataract patient includes a detailed history, a comprehensive ophthalmic assessment, and discussion of the natural history of the condition, expected recovery, and potential risks. Presence of systemic co-morbidities such as uncontrolled diabetes, hypertension or unstable angina should be sought. The surgeon also pays attention to the presence of a neck deformity or abnormal posture, significant head tremor, or claustrophobia – factors which may affect patient positioning intra-operatively.
Routine preoperative laboratory testing is not indicated, and discontinuation of antiplatelet agents or anticoagulants prior to cataract surgery is generally not required. While several studies demonstrate a higher risk of subconjunctival haemorrhage, current available evidence does not support an increased risk of vision-threatening complications in association with these agents.
During the pre-operative assessment, the ophthalmologist routinely assesses the possibility of intra-operative floppy iris syndrome, which is strongly associated with the use of systemic alpha-1 antagonists, most commonly for symptomatic treatment of benign prostatic hyperplasia. Floppy iris syndrome results in progressive pupillary constriction during cataract surgery with possible prolapse of the iris through the corneal incisions, and is associated with a higher risk of intra-operative complications.
However, it can be safely managed with additional measures that maintain pupillary dilation during surgery. It is important to note that discontinuing alpha-1 antagonists preoperatively does not prevent floppy iris syndrome, which may occur long after drug cessation.
INTRAOCULAR LENS power CALCULATION
Modern-day cataract surgery is a very precise operation. Patients routinely expect and demand predictable refractive outcomes, and desire reduced dependence on spectacles post-operatively. Knowledge of the patient’s vision requirements, hobbies, and personality are crucial in selecting an appropriate intraocular lens and an optimal refractive outcome.
Accurate measurement of the eye’s axial length and central corneal power, combined with the selection of an appropriate intraocular lens implant, based on a power calculation formula, is the minimal requirement to achieve the targeted postoperative refraction. This is done preoperatively using a high-resolution non-contact optical biometer, which uses a laser to make precise measurements of the eye. Modern intraocular lenses have an in-built UV filter, as well as aspheric optics. The latter improves mesopic (low light condition) and scotopic (dark condition) contrast sensitivity and visual quality by reducing optical aberrations of the eye.
Modern day implants also correct the patient’s underlying refractive error (short-sightedness, long-sightedness, and astigmatism). Additionally, use of presbyopia-correcting IOLs (multifocal or extended focus lenses), or monovision may improve quality of life by reducing glasses dependence after cataract surgery.
Monovision involves correction of one eye for distance vision and the other eye for intermediate or near vision. The success of monovision depends on blur suppression, where the blurred image from one eye does not interfere with the image from the in-focus eye. Patients with a history of successful adaptation to monovision with eyeglasses or contacts lenses are particularly well suited for this modality.
However, both multifocal and monovision techniques come with some optical side effects and whether the reduced dependence on glasses outweighs these side effects will vary between patients, making careful and considered patient selection a critical step of successful cataract surgery.

SURGICAL TECHNIQUE
Cataract surgery is generally completed as a day procedure under local or topical anaesthesia. Intravenous sedation is commonly used to complement the anaesthesia in order to optimise the patient’s surgical experience and cooperation.
The operation generally takes 15 to 20 minutes to perform, and is associated with minimal to no post-operative pain. In many cases, the patient’s vision is improved even at the first post-operative day, but continues to sharpen further over a few days.
A recent adjunctive tool used in cataract extraction is a femtosecond laser, which can be used to construct the corneal incisions and to perform some of the steps in cataract surgery including opening of the lens capsule and cleaving of the cataract. There is still controversy around the relative benefits and disadvantages of laser-assisted cataract surgery, and while it is associated with more reproducible wounds and more predictable lens centration, this is yet to translate to a meaningful clinical benefit for the patient. At present and as a relatively new technology, it is also associated with a significant financial cost that is borne directly by patients, although this may change in the future.
As with any operation, risks exist. Post-operative endophthalmitis (infection of the whole globe), although rare, is a potentially serious complication, occurring most commonly at three to five days post-operatively. It results in profound and rapid vision loss that may become permanent if not urgently treated.
The clinical triad of a red eye, severe vision loss and significant eye pain (not irritation) in the context of recent cataract surgery, should alert the general practitioner to the possibility of endophthalmitis and the patient should be referred immediately to the ophthalmologist or to a specialist unit for urgent assessment and treatment i.e. a vitreous biopsy for microbial culture and intravitreal injection of antibiotics.
In summary, cataract is an almost universal finding in the elderly population, but also affects younger age groups, especially diabetic patients and those taking long-term corticosteroids. Symptoms or signs of cataracts should ideally be looked for in all patients over the age of 65 in the general practice setting and be referred for further assessment if visually significant symptoms exist.
Dr Dana Robaei is an ophthalmologist based in Sydney. Her expertise includes complex cataract surgery, corneal transplantation and diseases of the anterior segment of the eye