The tripled bulk billing incentive is making a difference, especially in rural and regional Australia.
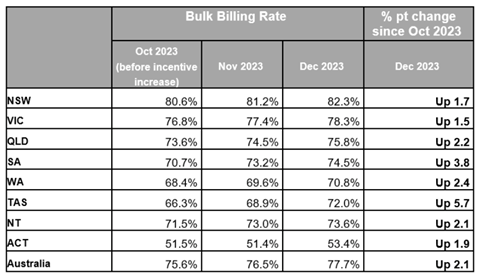
Data released to coincide with Medicare’s 40th birthday today reveals a 2.1 percentage point uptick in bulk billing in the two months immediately following the introduction of tripled bulk billing incentives.
In October, the month before the incentive increase, the national bulk billing rate had fallen to the lowest point since 2011, at just 75.6%.
It immediately rose to 76.5% in November and 77.7% in December.
Source: Office of Mark Butler, Minister for Health and Aged Care
It’s a small increase, but an uncharacteristically large one to have taken place over just two months, considering bulk billing rates have historically tended to vary by less than 1% each year.
Pre-pandemic, the rate had been slowly but steadily increasing, having sat at around 78% since 2016.
This increase accelerated in the 2020, 2021 and 2022 financial years, reaching a high-water mark of 82.2%, which was understood to be largely driven by telehealth and the covid-19 vaccine rollout.
According to data from the Productivity Commission’s Report on Government Services released yesterday, the government’s expenditure on general practice shot up and peaked in the 2020-21 financial year (when GP attendances also peaked) before a matching steep decline in the 2023 financial year.
The expenditure is still higher than before the pandemic, but dropped to the tune of $800m in one year alone.
The 2023 financial year was also when the bulk billing rate took a nosedive to 76.6%.
It’s this context that gives a 2.1 percentage point rise significance.
Related
Health Minister Mark Butler, along with the RACGP and AMA, have celebrated the turnaround.
“In the Hunter Valley, GP Dr Yasas Samarasinghe said it was a lifeline, and in the Northern Rivers of NSW another doctor told us that it’s going to encourage those that have recently changed to private billing to go back to bulk billing,” Mr Butler told the audience at a Medicare 40th birthday symposium today.
“And even in these early days, just a couple of months into the new incentives, that is exactly what we’re seeing right across the country. Clinics everywhere are making that shift.”
All states and territories recorded a rise in bulk billing over the November-December period, but the biggest jump was in Tasmania, where the rate rose by 5.7 percentage points.
Victoria had the smallest response of any jurisdiction, with an overall 1.5 percentage point increase, but regional and remote areas of the state reportedly recorded a five-percentage-point increase.
According to Mr Butler, more than half of the bulk billed appointments that have utilised the tripled incentive have been in non-metro areas.
“This is not just a benefit for the hip pocket of Australians living in those communities,” he said.
“It’s also important for their health.”
He also alluded to the possibility of more funding in store for general practice.
“The era of calculated neglect of our terrific universal health system is now over,” he said.
“A new era of strengthening Medicare has taken its place.”
The work, he said, has already begun to “to return our cherished Medicare to its rightful place as one of the world’s most envied public health systems”.
AMA president Professor Steve Robson called the early statistics an “encouraging sign” but called on the government to double down on the success by investing more money into primary care this year.
“We now have the early proof that investing in the right way in Medicare can deliver returns,” he said.
“There is more work to be done … Medicare has not kept up with the changing health environment … including through improved funding arrangements.”
Dr Nicole Higgins, RACGP president, also called for increased funding for the scheme.
“Just like Medicare, general practice and primary care is the foundation of our healthcare system,” she said.
“We need to invest in our footings – at the moment, they’re a bit crumbly and if we don’t do this, the rest of the system will fall over.
“Strengthening Medicare is a once-in-a-lifetime opportunity to change the system for better, and what we’ve seen with today’s data is that funding drives outcomes.
“If we want to have a strong general practice and primary care system and a strong health care system, we must fund it.”





