Is there any evidence they will be lost to allied health professionals more willing to embrace other funding models?
An interesting spat occurred this week when ASGP head Dr Chris Irwin wrote an open letter to the RACGP saying MyMedicare, rather than offer GPs more control through creating a tighter link to their patients, would encourage substitution of GP tasks within a practice, deplete individual GP income and take control away from GPs.
Dr Irwin, who describes MyMedicare as a “capitation” model of funding – perhaps cheekily in order to whip up a bit of fear and loathing – argues in his letter that embracing MyMedicare is playing into the government’s hands. Such a model of funding would loosen the relationship between a GP and their patient by diluting the transparent funding relationship in a fee for service model.
This he says would give the government more ability to introduce substitution of GP services via block funding practices to introduce various other allied health professionals into the mix.
Normally such a letter might have gone through to the keeper without the college bothering to try to play at it, but Dr Irwin upped the ante quite a bit by suggesting in the letter that college president Dr Nicole Higgins might have won the last college presidential election on a promise she has now broken.
“I believe the outcome of the last election would have been different if voters had known Dr Higgins would be endorsing MyMedicare to this extent,” the letter says. To be clear, Dr Higgins freely admits having shifted her position on the program, and there’s no suggestion she intended to mislead.
They might be fighting words – for the next election at least. Has the next campaign already started?
Dr Irwin contested the last election and won the primary vote by about 200 votes but lost in the run-off rounds. He’s not exactly an outside chance of winning next time.
Dr Irwin believes most GPs don’t support MyMedicare and called on the college to survey members and then review its position if it found that support was lacking.
Coincidentally, leading GP education provider HealthEd surveyed GPs on the very issue just a couple of weeks ago (with a huge sample size made up mostly of college members), and the results suggest that Dr Irwin might be right about GP support for MyMedicare.
While the survey didn’t ask the question “do you support MyMedicare?” directly (don’t worry, TMR is going to ask it at HealthEd’s next survey on 14 November for absolute clarity) it did ask a pretty good proxy question, is “MyMedicare likely to have sufficient engagement from practices or patients to be successful?”.
Sixty-eight percent of respondents said no. Ouch.
In the same survey 55% of respondent practice owners said they had already registered (39%) or intended to (16%).
In the context of the main result this is likely less an endorsement of the program and more practices optimising any potential for additional income, which is probably another question someone should ask.
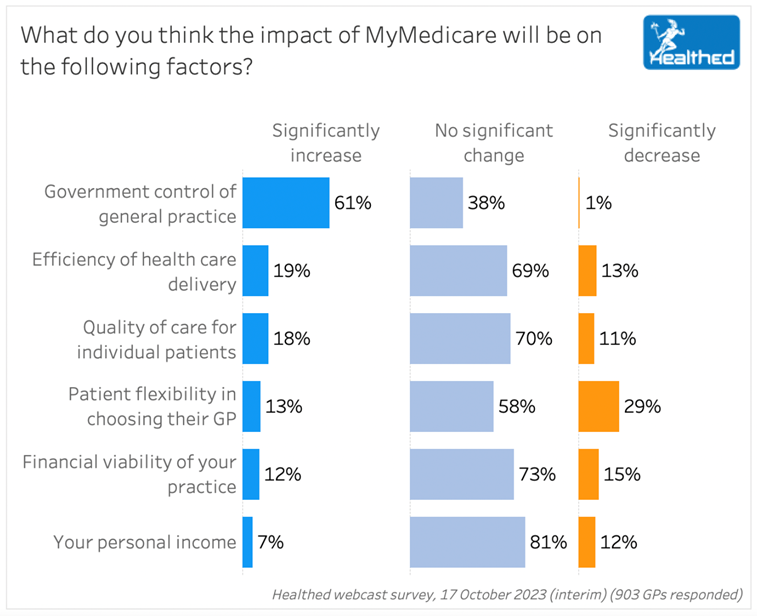
Possibly more telling for Dr Irwin, the college and the federal government is what individual GPs think about MyMedicare in terms of whether it will increase government control of general practice, increase efficiency of healthcare delivery and, ultimately, increase the quality of care for their patients.
The college and the government aren’t likely to be encouraged by the results of this question (below) which probably is enough for anyone to conclude that overwhelmingly GPs don’t believe in MyMedicare at all so far.
Still, who cares what GPs actually think, right? It’s impossible for them get the bigger picture from where they are all standing (the coalface, where things actually happen) but they will no doubt be pleasantly surprised after the fact at just how great an idea MyMedicare ended up being for them.
They just need to breathe in a little and have a little faith.
Or not.
Despite my ironic tone here, I’m not necessarily siding entirely with GPs in what so far seems to be a pretty clear dismissal of the MyMedicare concept.
Its intention isn’t terrible.
It’s aiming at a mixed funding model (more outcomes-based funding in the mix) that supports more continuity of care at the primary care level mainly through GPs.
But between this broad and possibly admirable goal and the plan so far, anyone wanting this to work should be worried about where GPs are going to find that “little faith”, and what is going to happen if GPs mechanically sign up – leading to a possibly false impression they support it – just in case they can get a few more dollars.
If they remain entirely dismissive of the idea, which so far they seem to be, that isn’t going to be good for implementation of the program, no matter what anyone thinks in government about having to push through to the other side.
Speaking at a webinar in September, Dr Higgins said she had gone from a MyMedicare sceptic to believing it would be “one of the most important drivers for general practice going forward”.
“I’m going to be a little bit crude … if we don’t [register our patients], somebody else will,” she said.
“I think it’s really important that we make sure that we bring our patients with us in general practice and provide that continuity of care.
“Because if we don’t, the system will fragment and there are going to be other options about how that care gets delivered, potentially through the reforms that are coming.”
It’s a suggestion GPs should “lock in” their patients through MyMedicare in order to stop them from being poached by other allied professions who will likely rush to embrace any funding that pushes some of the money their way.
Broken record, I’m not a GP so what would I understand or know, but …
What’s the logic here, or indeed the evidence, that signing up a patient formally to your practice or yourself will bind them to you in any more meaningful way than they are bound already?
A GP I know reasonably well, who is still a pretty big deal in GP and government circles, said to me the other day “Jeremy, everyone hates GPs, but virtually no one hates their own GP … think about that.”
I did. My first thought was, “Yeah, I love my GP … she really understands me (not easy) and I trust her quite a bit.” (I don’t trust many sentient beings outside my wife, kids and Labrador.)
I think what this GP was telling me was that a lot of people – government included – are underestimating the “lock” that a lot of GPs already have with their patients through providing them with pretty good long-term care.
Without bodies like BEACH, really important data around stuff like this, is pretty hard to get and understand these days. It’s still baffling why for a measly million bucks a year the government doesn’t refund BEACH or an equivalent program, so they can understand important stuff like this much better and stop guessing what GPs think.
To awkwardly provide some sort of business analogy – I run a business so I’m arguing that gives me some ability to comment – when I sign important contracts with suppliers or customers of my business, much to the dismay of my accountant, I pay virtually no attention to the actual words or intentions of the contract – I go to the signing part straight away (much easier these days with Docusign).
The reason is that I’ve already made my decision based on the actual relationship I have with that customer or supplier and I trust that signing will be OK – saves me a lot of time reading long-winded ridiculously constructed contracts that I never understand legally anyway.
It’s cuts both ways – do I have a trusting relationship and good track record with that customer or supplier?
When things go wrong contracts never help you much and inevitably when you look back you can see in how you engaged with that party why things went off the rails.
Just spitballing (as always) here, but don’t most good GPs already have a really good contract with a large proportion of their patients? Not a written transactional contract for sure, but a contract of sorts none the less, one that also works both ways?
As a GP what do you think?
If that’s the case then what is MyMedicare really trying to do – for GPs, for the government and for patients?
I’m struggling to figure that out at this point of time.
If GPs are too, which they seem to be, we surely have a problem that government should think a little more carefully about.
Whatever the actual value proposition is, it’s going to need to be much better defined for GPs before you get them on board in spirit, which the government almost certainly is going to need if they really want it to work.