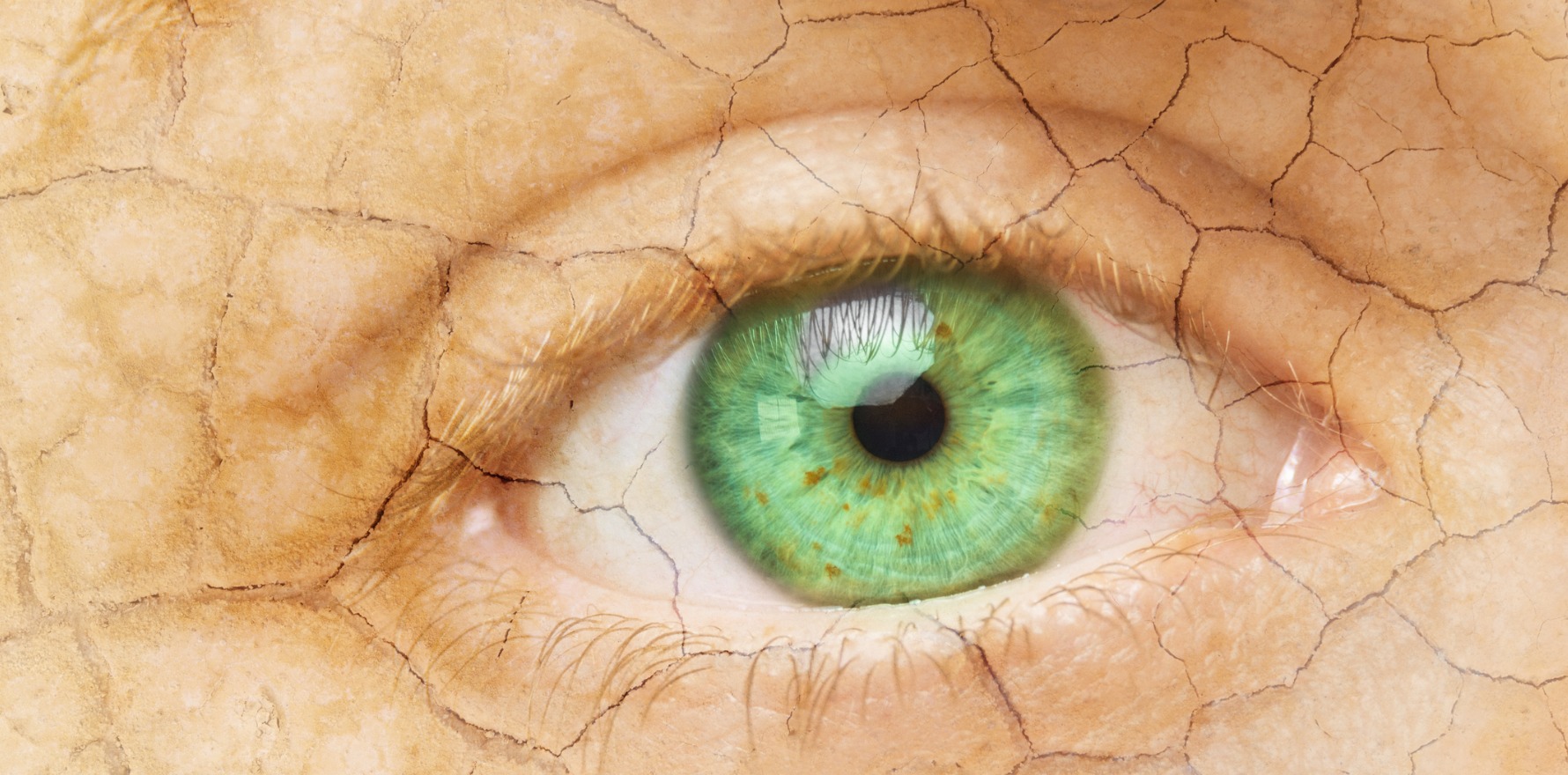
The common condition is often missed and left untreated, which can have significant long-term consequences.
Eyedrops, good eyelid hygiene and fish oil tablets can go a long way to treating dry eye in menopause, according to one expert.
Dry eye disease can significantly reduce quality of life and, if left untreated, may eventually cause vision loss. Older age and female gender are known risk factors for dry eye, meaning women experiencing menopause are prime candidates for the condition. However, dry eyes in menopause are frequently missed and infrequently treated.
As part of his plenary presentation at the Australasian Menopause Society in New Zealand last month, Dr Andrew Logan, a Wellington-based ophthalmologist, shared some expert tips in how to identify and manage dry eyes.
“Studies have shown the prevalence in the overall population is between 7% and 34%, [but dry eye is] up to two times more frequent in older women than in older men,” Dr Logan told delegates, before suggesting changes in hormone levels were likely to underlie the increased risk.
“Dry eyes are more common in pregnancy and with oral contraceptive use [where oestrogen levels are increased] as well as in menopause [where oestrogen levels decline],” said Dr Logan.
The hormonal changes in menopause results in chronic low-grade inflammation in the lacrimal glad, which reduces tear secretion. In turn, the reduced tear secretion leads to an increased concentration of electrolytes in the tears that are produced, which subsequently damages mucin-producing goblet cells and further inflames the lacrimal gland, according to Dr Logan.
“It’s a vicious circle where each step aggravates the next one. [But] the great thing is that each of these steps offers the opportunity for intervention, which may help reduce the inflammation and the associated symptoms,” Dr Logan told delegates.
While ophthalmologists have access to several tools to help diagnose dry eye, Dr Logan recommended non-ophthalmologists focus on the clinical history and symptoms and use one of the many available questionnaires, such as the Standard Patient Evaluation of Eye Dryness (SPEED) Questionnaire, to gauge how severe the condition is and whether patients are responding to therapy.
Common symptoms of dry eye include a stinging or burning of the eye, episodes of blurred vision, heavy eyelids, an inability to cry when emotionally stressed, discomfort wearing contact lenses and, counterintuitively, episodes of excess tears following periods of very dry eyes.
Despite the proposed role of menopause-related hormone changes underlying dry eye, evidence suggests MHT may make dry eye symptoms worse by exacerbating meibomian gland dysfunction, which negatively affects tear flow. On the flip side, systemic or local androgen-based therapies may be a more effective treatment as they upregulate meibomian gland activity.
Dr Logan recommended a simple, three-pronged approach to treating dry eye regardless of the patient’s age and gender:
- Restoring appropriate ocular lubrication using preservative-free artificial tears or eye drops,
- Commencing fish-based omega-3 supplements, and
- Improving eyelid hygiene by reducing or stopping use of mascara and eyeliner and/or using cleansing wipes on a regular basis to preference interference with meibomian orifice and gland function.
“This trio of simple, non-invasive therapies may help confirm the diagnosis and may be sufficient to get the patient out of trouble. If symptoms persist, then it’s worth referring to an optometrist or ophthalmologist,” Dr Logan said.
The more advanced treatments available to eye specialists include placing punctal plugs (small silicon or polymer inserts) into the eyelid, as well as topical anti-inflammatory and cyclosporine treatments.