We should support each other’s small businesses by paying GP gap fees ourselves.
I’d like to share some reflections on my money mindset, as I’m hearing from some of you that they are helping you in making the necessary changes, given the Medicare and GP crises.
None of us is doing this alone but it can feel very lonely in the midst of it.
Since 2021, I’ve been following several leaders in other industries that do not have a Medicare safety net for paying their overheads.
As more and more of us are abandoning bulk billing, for a variety of reasons touched on in previous articles, it’s giving permission for those of us still hesitating to do likewise. There’s never been a better time to make the jump.
I left UBB in 2013 as a final term GP registrar. Nonetheless, despite a decade of mostly private billing, I’m still occasionally uneasy at the idea of talking money with patients; I still hesitate to enforce a late cancellation fee, or am tempted to discount a consultation or procedure even though I know my business can’t take it.
But I am getting better at it. I press pause when these feelings overwhelm me; I think about whether it’s a reaction to something someone has actually said, or a genuine desire to do a favour “this time”, and then proceed. I watch my tendency to offer unsolicited discounts because someone mentions how hard rising costs are on them at them moment – they knew the fee when they booked to see me, presumably they’re not asking for a discount, but debriefing; they’re an adult and can advocate for themselves without my jumping in to rescue them.
I’m better at self-soothing and managing my anxiety around talking money and being seen potentially as “greedy”. And I’m better at letting those who decide they don’t wish to, or can’t pay my fees, go elsewhere – in fact, it was far easier when I was co-located with BB drs back in 2013, within the same practice that I could refer patients to.
This week I had an appointment with my old GP, the one who was so helpful during a very difficult period of my life, whom I’d not had occasion to see since 2019.
Despite her practice being mixed billing even back then and my asking to pay the gap, she’d refuse. This resulted in the unintended effect that I’d rarely go to see her, seeing the appointment as a waste of her time that she could’ve filled with a full-fee-paying patient instead.
With the current Medicare crisis, I went armed with new reasons as to why she should bill me, including my last-resort comment: “If you won’t charge me, I’ll find another GP.”
Fortunately for me, she capitulated, but she may have nonetheless been uneasy about it, as she noted to reception about privately billing me “she’s insisting”. Which is OK!
We need constant reminders to value ourselves, our skills and our time, and that we are not greedy for doing so.
In my own clinic, we’ve raised fees appropriately, we charge late-cancellation and no-show fees and my staff are now so well trained I don’t even have to get involved. Last week when I was inclined to waive a late-cancellation fee (two hours’ notice), staff said to me “what’s the point of a policy if you won’t uphold it?” Touché.
An FRACGP colleague recently asked me for help wording her late-cancellation policy, given at least one or two patients cancel each day and she’s booked out till late April. This is another area where we need to be firm – just ask restaurants.
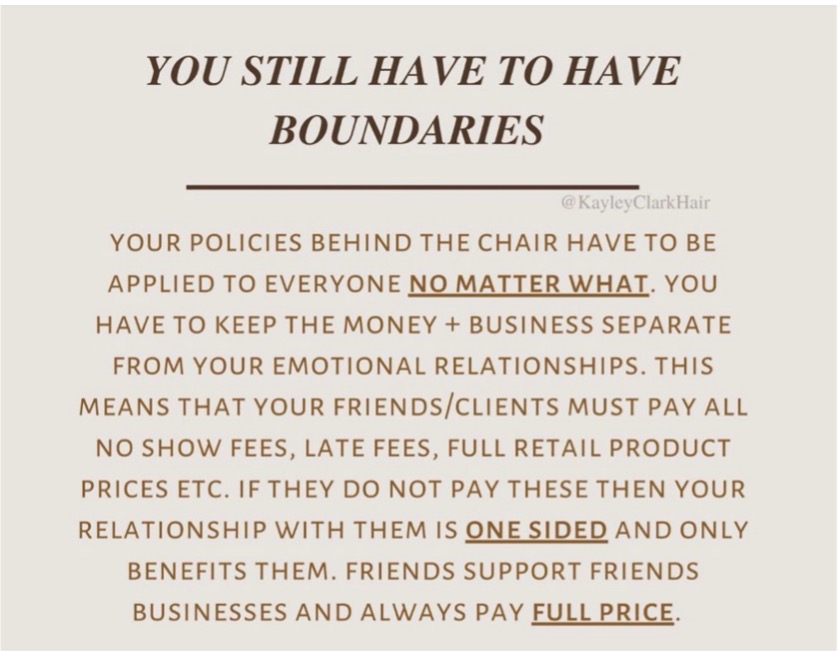
We can learn a lot from other industries. A hairstylist I follow on social media posted recently:
And while I know there will always be those among us who feel for any number of reasons that to charge is to sell out, or to do medicine for the wrong reasons, I think it’s high time for a reset.
For the longest time in medicine, we’ve afforded each other the professional courtesy of not charging gaps to see each other as patients. For years, I’ve been part of a miniority of GPs arguing against this, citing that what may have worked for our colleagues who are close to retirement or retired, no longer works for us. The traditional model of doctors hailing from well-to-do doctor families no longer holds true; many of us are single parents; others are in marriages where we’re the sole income earner; yet others have additional needs and debts.
Even if we come from well-off families, none of us signed up to medicine to be charities, and the idea that discounting or working for free is “good” is outdated and exploitative.
Since 2016, I’ve always had a significant number of colleagues as patients, from all walks of the field; it was then that I made the difficult decision to stop discounting and bulk billing them because the work I did then, as now, is neither fast nor easy. My patients to this day know I don’t discount or do mates’ rates, and I won’t be offended if they’d prefer to see someone who will, it just won’t be me.
Once my policies are in place, I’ve found that what I need to work on are getting staff on board, and then soothing my own anxiety every time it flares. Lastly, it’s about educating patients around expectations and then following through on the policies.
Recently we raised the fees for a Level B on a Saturday above the weekday fee. Staff informed patients when booking, explaining that while the rebate would remain the same, the fee went up to accommodate the higher costs of running the practice out of hours. No one complained, people accepted it.
Similarly, when fees went up in February this year in line with inflation, we notified all patients when booking, with a reminder at the end of the appointment. With inflation hitting the cost of just about everything, small business owners are dealing with two price crises: in their business and in their personal lives, like everyone else. It would be madness to continue to absorb this cost out of a misguided sense of duty.
No one doubts that we care for our patients and want good for them. Equally, I don’t know a single doctor who charges gap fees who doesn’t also do pro bono work, either in the same clinic or elsewhere, for the genuinely disadvantaged. It’s important to recognise that many of our ideas around Medicare, including professional courtesy, are outdated and that in clinging to them we may be doing more harm than good to the speciality we are trying to save.
The younger doctors willing to consider general practice don’t want to carry the can for government failure. They want career satisfaction and pay parity with their non-GP colleagues. Many are comfortable charging gap fees but limited by clinic owners who insist they bulk bill for fear of losing business.
Friends support friends’ businesses.
We pay proper fees and insist on doing so, without expectation of handouts, including late fees.
If we want our speciality to be great again, it must begin with us, our attitude towards each other and we must want good for each other including in our pay.
Dr Imaan Joshi is a Sydney GP; she tweets @imaanjoshi.





