What’s new in the work up and management of peripheral nerve injury, including the latest diagnostic advances
Peripheral nerve injury is common in clinical practice and can be the result of entrapment, chronic or repeated trauma, compression from anomalous structures, or acute trauma.
Of these mechanisms, extrinsic compression and entrapment are most common.1
What nerve is injured?
A decent clinical history and examination will usually enable a clinician to accurately diagnose the nerve or nerves involved. However, there are a number of traps in the clinical presentation that can divert attention away from the true source of the symptoms.
These red herrings include:
• Distal peripheral nerve injuries may be associated with proximal symptoms. The classic example is carpal tunnel syndrome which is frequently associated with symptoms proximal to the wrist and hand. This, combined with the high rate of asymptomatic cervical spine neural foraminal stenosis seen on MRI in older individuals, can often mislead clinicians into considering cervical radiculopathy as the diagnosis. Where there is any doubt as to the origin of neuropathic limb symptoms, always exclude a peripheral source before recommending a spinal intervention.
• Not all nerve injuries present with “textbook” symptoms. This may be due to partial nerve involvement and anatomical variations. For example, patients with peroneal neuropathy may not have sensory symptoms. And conversely, entrapment or injury of some motor nerves, such as the posterior interosseous, obturator and suprascapular nerves may initially present with limb pain but no significant weakness.
• Patients may have overlapping syndromes complicating the clinical presentation, for example, carpal tunnel syndrome superimposed on the peripheral polyneuropathy of diabetes mellitus, or mixed radiculopathy and peripheral nerve injury.
Where and why?
Once the suspect nerve or nerves have been identified on clinical grounds, the next step is confirming the location of the lesion. Clinical examination will usually provide some localising clues although it is best to supplement this with more objective investigations, particularly as these may also provide additional information regarding the mechanism and severity of the injury.
Electrodiagnostic studies
These include nerve conduction studies and electromyography and are critical to adequately assess the severity of nerve injury as well as providing localising and pathophysiological information regarding the injury. Reduced or absent motor or sensory responses, seen on nerve conduction studies generally indicate loss of axons.
Focal slowing of motor or sensory nerve conduction indicates demyelination in the segment being tested. The precise location of the lesion can be further refined using “inching” studies, where stimuli are delivered to the nerve over multiple short segments, usually 2 to 3cm apart.
Electromyography(EMG) can be helpful in three ways. It can detect fibrillations, which suggest that there are muscle fibres without a nerve supply and indicate active denervation. Active denervation is seen within one to three weeks after axonal injury and may persist in injuries where complete reinnervation has not yet taken place.
EMG also allows assessment of the motor unit morphology which can give clues as to whether reinnervation is occurring and where the person is in this process. The motor unit changes with reinnervation such that the unit initially becomes more broad and complex before reorganising into a larger-amplitude and usually longer duration unit with time. Neurogenic motor unit changes on EMG indicate that there has been reinnervation following axonal injury.
Finally, analysis of motor unit recruitment with increasing voluntary effort can provide further information regarding nerve injury. If EMG indicates that recruitment of motor units is reduced, it is likely there is failed conduction through motor axons because of either axonal injury or focal demyelination.
Imaging studies
• Neuromuscular ultrasound
Recent advances in ultrasound technology, specifically the introduction of higher frequency linear probes, has facilitated an explosion of research in peripheral nerve ultrasound.2
Details of a superficial peripheral nerve’s internal characteristics, such as nerve fascicles, can now be imaged using standard equipment. Ultrasound has the highest spatial resolution of all imaging techniques.
A normal nerve demonstrates a “honeycomb” appearance due to dark (hypoechoic) fascicles surrounded by light (hyperechoic) perineural fibrous tissue.
A chronically injured nerve will change the ultrasound appearance in predictable ways irrespective of the mechanism of injury.
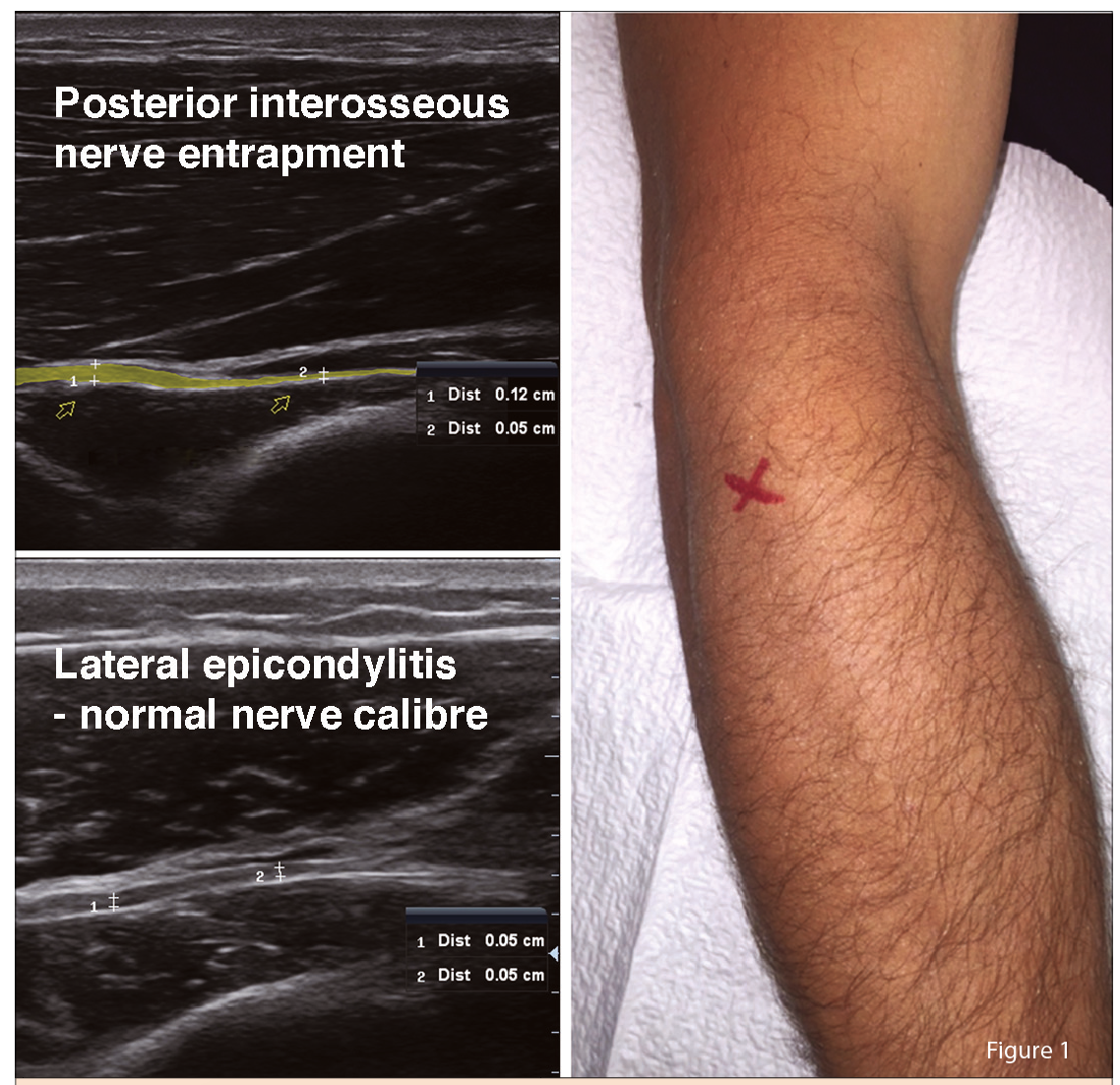
On ultrasound, injured nerves appear larger which can be determined by measuring thickness or cross sectional area (See Figure 1, above).
A chronically injured nerve also loses definition of its internal architecture such that the nerve is more uniformly hypoechoic (darker) on ultrasound.
By adding ultrasound to the electrodiagnostic examination, anatomical information is obtained which will help with the precise localisation of the nerve injury as well as providing clues as to the mechanism of the injury. For example, entrapment of the nerve in a fibrous tunnel may be confirmed, or an anomalous anatomical structure causing nerve compression may be identified.
A major advantage of ultrasound is that many devices are now portable and thus can be employed in the clinic setting, at the time of clinical or electrodiagnostic examination.
There are a small but increasing number of neurologists in Australia who perform neuromuscular ultrasound, and they are well placed to integrate this technology into the diagnosis of nerve injury.
The earlier surgical intervention is undertaken in severe injuries the better the subsequent outcome.
MR neurography
MRI is a powerful tool for imaging of soft tissues including peripheral nerve. The development of new protocols and sequences has facilitated high resolution imaging of peripheral nerves.
MR neurography studies usually include at least one T1-weighted sequence which shows anatomical detail well. In addition there should be a fat-suppressed image (either T2-weighted or short tau inversion recovery [STIR] sequence), which shows water-based pathologies well, such as nerve inflammation and oedema.3
MRI has advantages over ultrasound in terms of sensitivity to subtle pathology and the ability to use multiple sequences to delineate different types of nerve pathology. However, MRI is time consuming and expensive and some patients find the actual procedure claustrophobic and intolerable.
Should electrodiagnostic studies or imaging be the first-line diagnostic study?
Electrodiagnostic studies have been the mainstay in the diagnosis of peripheral nerve injury for many years.
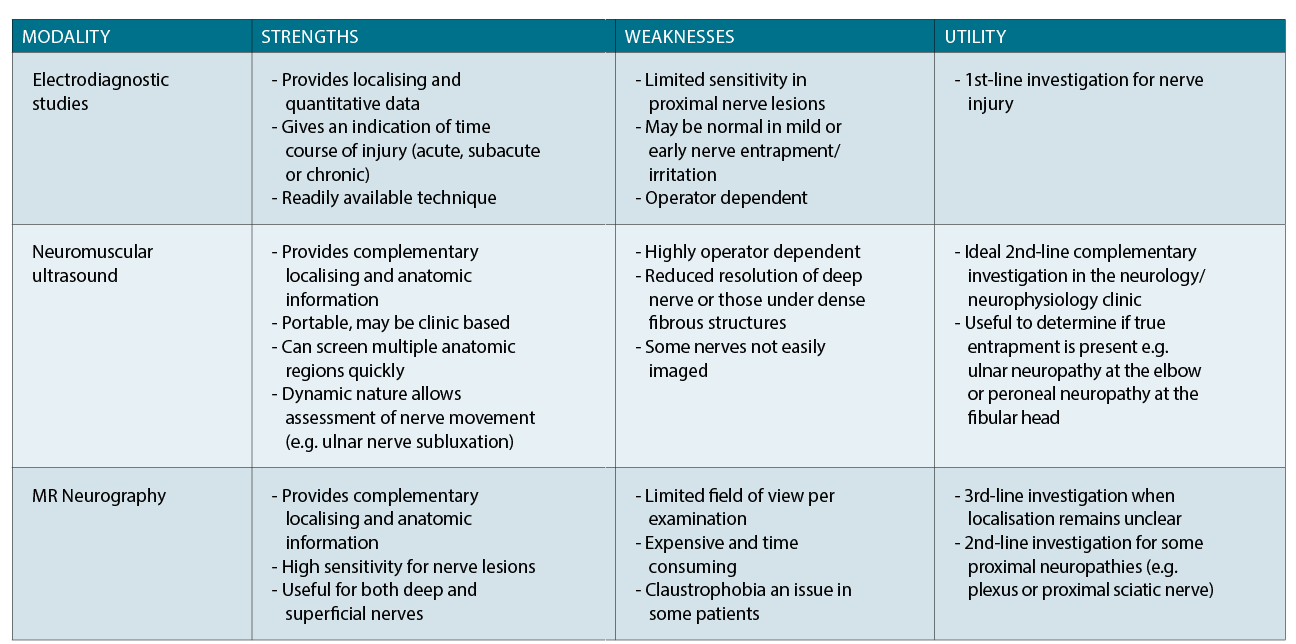
However, in the last several years both ultrasound and MRI have become increasingly incorporated in the complete work up of some patients, with each modality demonstrating specific strengths and weaknesses (See
table 1, above). In some patients both imaging modalities may be needed to obtain a complete set of diagnostic information.
The main drawback of imaging is that it does not adequately grade the severity of the nerve lesion and as such electrodiagnostic studies remain invaluable for the work up of nerve injury and are unlikely to be replaced by imaging in the medium term.
However, sensitivity of electrodiagnostic studies is limited in some nerve injuries, in particular those involving proximal nerves or when nerve injury is mild.
In addition, electrodiagnostic studies may fail to localise the lesion to a precise nerve segment, which may be necessary to optimally target treatment.
Currently electrodiagnostic studies are recommended as the first-line investigation for patients with nerve injury, with imaging considered in cases where electrodiagnostic studies are negative or where complementary anatomical information is required.
Grades of nerve injury
Determining the grade of the nerve injury is critical to the prognosis of spontaneous recovery as well as guiding appropriate treatment.
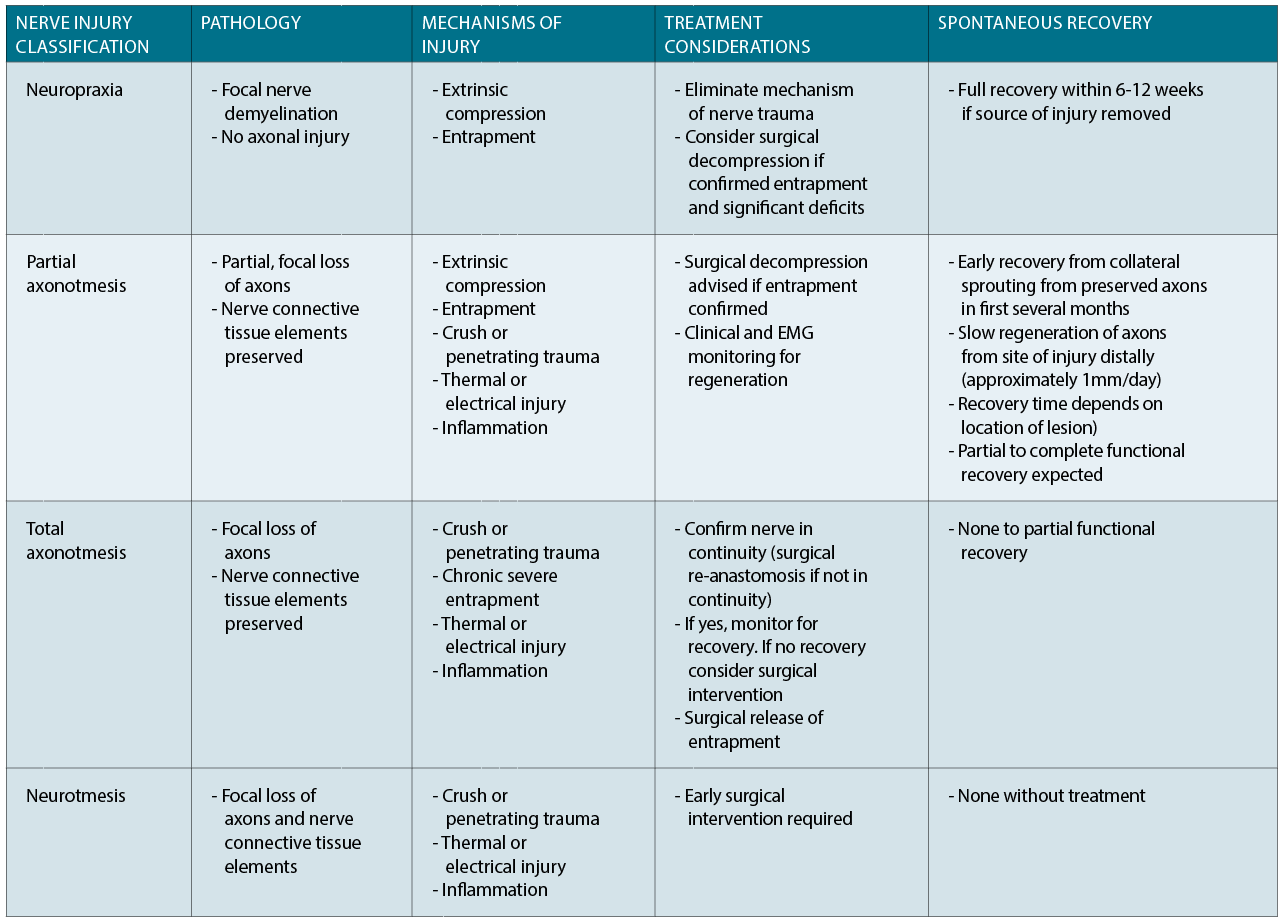
The most well-known classification of nerve injury was proposed by Sir Herbert Seddon. This classification system serves as a reasonable guide as to which treatment options may best benefit the patient and help predict the likelihood of spontaneous recovery.
There are three categories: neuropraxia; axonotmesis; and neurotmesis (See table 2).
Differentiating between neuropraxia and other grades of nerve injury is relatively straightforward.
Nerve conduction studies show focal slowing at the level of the lesion with or without conduction block (normal amplitude produced by stimulating below the nerve lesion and reduced response amplitude with stimulation above the lesion).
EMG will be normal besides reduced motor unit recruitment.
Differentiating between total axonotmesis and neurotmesis is difficult, particularly when the nerve remains in continuity. Nerve conduction studies and EMG will be identical in both and presently there is no diagnostic study that can distinguish these two grades early in the course of the injury. Making the distinction is very important, as neurotmesis will never recover without surgical intervention to resect the injured segment and reconnect the ends or apply a nerve graft, while an axonotmetic injury may recover spontaneously.
In addition, the earlier surgical intervention is undertaken in severe injuries the better the subsequent outcome. Conversely, a severe axonotmetic injury destined for spontaneous recovery will recover better without surgical intervention.4
At present, in a nerve lesion where continuity is confirmed, the recommended approach is to wait for signs of spontaneous recovery. If recovery has not occurred after several months, surgical exploration with intraoperative nerve conduction studies (compound nerve action potentials) is a standard approach to detect any regenerating axons across the injured segment. However, access to this technique is extremely limited in Australia.
Some research groups have been developing a novel MRI technique (diffusion tensor tractography) capable of detecting axonal regeneration, which with further refinement may provide a non-invasive way of monitoring nerve regeneration.5
Treatment options
Like all aspects of medicine, the treatment must be matched to the disease.
In mild cases of extrinsic nerve compression or entrapment, avoidance of activities that may be causing ongoing nerve injury, as well as nerve gliding exercises and splinting may be sufficient to manage the symptoms.
Corticosteroid injections with or without local anaesthetic are a valuable option for patients with significant symptoms of nerve entrapment, particularly when associated with pain. Carpal tunnel syndrome is the most effectively controlled with local corticosteroid treatment although the benefit of this treatment rarely exceeds three months.
Other entrapment neuropathies or painful mononeuropathies may also benefit from local corticosteroid treatment, and risks are generally low. Ultrasound-guided injections are recommended over blind injections to avoid iatrogenic nerve injury. CT-guidance may be necessary for deep injections, such as the sciatic nerve at piriformis.
Surgical intervention is over-utilised in some situations, particularly in mild intermittent carpal tunnel syndrome and mild ulnar neuropathy.
Surgery is a very effective treatment for neuropathies where a nerve has become entrapped in a fibrous or fibromuscular tunnel. This is the case in the vast majority of patients with carpal tunnel syndrome, but is less common in ulnar neuropathy and uncommon in peroneal neuropathy at the fibular head.6
Careful work up of a nerve injury as described above will enable patients to be appropriately triaged to surgical or non-invasive treatment options.
Dr Neil G Simon is a consultant neurologist, clinical neurophysiologist and neuromuscular ultrasound practitioner. He is principal neurologist, Northern Beaches Neurology, Dee Why; and staff specialist, St Vincent’s Hospital, Sydney
References
1. Simon NG, Kiernan MC. Mononeuropathy. In: Hilton-Jones D, Turner MR, eds. Oxford Textbook of Neuromuscular Disorders. Oxford: Oxford University Press, 2014: 93-114.
2. Gallardo E, Noto Y, Simon NG. Ultrasound in the diagnosis of peripheral neuropathy: structure meets function in the neuromuscular clinic. J Neurol Neurosurg Psychiatry. 2015 86: 1066-1074.
3. Simon NG, Talbott J, Chin CT, Kliot M. Peripheral nerve imaging. Handb Clin Neurol. 2016 136: 811-826.
4. Simon NG, Spinner R, Kline DG, Kliot M. Advances in the neurological and neurosurgical management of peripheral nerve trauma. J Neurol Neurosurg Psychiatry. 2015 87: 198-208.
5. Simon NG, Narvid J, Cage T, et al. Visualizing axon regeneration after peripheral nerve injury with magnetic resonance tractography. Neurology. 2014 83: 1382-1384.
6. Stewart JD. Foot drop: where, why and what to do? Pract Neurol. 2008 8: 158-169.