Underprepared and undersupported hospitals are a ‘ticking time bomb’ in the COVID-19 pandemic, the RDAA and ACRRM have warned
Thanks for visiting The Medical Republic‘s live COVID-19 blog.
And thanks to our sponsor and supporter for funding this project with an independent grant, Boehringer Ingelheim.
The latest
- COVID-19 and air-pollution: a complicated relationship.
- Underprepared and underresourced rural/remote hospitals a ‘ticking time bomb’, RDAA warns.
- No evidence for faster viral RNA clearance with antiviral drugs, study finds.
4.35pm, 15 April
- And for those of us still struggling to buy toilet paper and hand sanitiser, here is a lovely, shining moment of schadenfreude to bask in, courtesy of ABC News. An Adelaide man has tried – and failed – to return around $10,000-worth of bog roll and hand sanitiser to a local supermarket after using a team of people to stockpile them at the start of the pandemic but being blocked from reselling them online.
That’s 132 packs of toilet rolls and 150 one-litre bottles of sanitiser.
Please excuse my smirk.
- The multi-layered interaction between air pollution and COVID-19 has generated some interesting findings.
First there was a US study that compared COVID-19 death rates with long-term average exposure to fine particulate matter across around 3000 counties. It suggested that an increase of just one microgram per cubic metre of PM2.5 was associated with a significant 15% increase in COVID-19 death rates. (And aren’t we glad this pandemic didn’t hit during the bushfires).
Now there’s evidence that the COVID-19 pandemic is actually reducing air pollution levels because of reduced human activity, and that in turn could be avoiding deaths.
This new study, published on preprint server MedRxiv, used satellite and ground-level air pollution data for 27 countries to show that ground-level nitrogen dioxide levels – produced by fossil fuel combustion – dropped by 29% and fine particulate matter levels declined by 9% during February/March compared to the same time last year.
Based on this, they estimated that 7400 premature deaths and 6600 cases of paediatric asthma were avoided in the first two weeks of lock-downs. By six months, if these reductions in pollutant concentrations are maintained, 780,000 premature deaths and 1.6 million cases of paediatric asthma could be avoided globally.
“While the state of global lockdown is not sustainable, these findings illustrate the potential health benefits gained from reducing ‘business as usual’ air pollutant emissions from economic activities,” they wrote.
- Underprepared and undersupported hospitals are a ‘ticking time bomb’ in the COVID-19 pandemic, the Rural Doctors Association of Australia and the Australian College of Rural and Remote Medicine have warned.
The two organisations expressed concerns about lack of PPE supplies and preparedness – such as simulation activities – in many rural and remote hospitals,
“For any small rural hospital which has not yet participated in simulation activities, or placed orders for the appropriate supplies, that clock is ticking,” said RDAA President Dr John Hall in a statement.
Meanwhile, a study of intensive care units across New York City has found that the number of patients on ventilators increased nearly 2.5-fold, and the median severity of illness increased 40-fold from March 23 to April 6.
The paper, published in preprint server MedRxiv, showed that over that two-week period, average hourly occupancy of ICU beds in 14 ICUs and nine hospitals increased from 64% to 78% and the percentage of intubated patients increased from nearly 34% to 84%.
Researchers noted that the median severity of illness score increased from 1.08 to 39.38, which translated to more than an eight-fold increase in mortality risk.
- Antiviral drugs do not appear to speed up viral clearance in patients with COVID-19, according to a retrospective study published on the preprint server MedRxiv.
The study of 284 consecutive patients admitted to Guangzhou Eighth People’s Hospital with COVID-19 found none of the antiviral regimens being taken by patients were associated with improved viral RNA clearance.
Thirty-six patients (12.7%) were taking oseltamivir, just over a quarter were taking lopinavir/ritonavir and just under a quarter were taking arbidol. In fact the study suggested that use of lopinavir/ritonavir was associated with slower clearance of viral RNA even after adjusting for potential confounders such as disease severity.
One-third of patients in the study cleared the virus – defined as two sequential negative tests on respiratory tract samples collected more than 24 hours apart – within 14 days, and nearly 90% had cleared it within 21 days.
“These data suggested that isolation for at least 21 days after the onset of symptom or first positive PCR test is warranted in both patients without or with improving symptoms,” the authors wrote.
- Symptoms in children infected with SARS-CoV-2 ‘differ wildly’ from those in adults, particularly the rates of fever, cough, pneumonia and lymphopaenia, according to a systematic review.
The paper, published on the preprint server MedRxiv – and just a reminder, these preprint papers are not peer-reviewed – analysed 38 studies involving 1124 cases of RT-PCR-confirmed COVID-19 in patients aged under 18 years. They found around one in seven patients were asymptomatic, one third only had mild symptoms, nearly half had moderate symptoms, and only 1.2% were critical.
Just over one-third of patients were diagnosed with pneumonia, and around 10% were diagnosed with upper airway infections. Fever and cough were the most common symptoms but only presented in around 48% and 42% of patients respectively.
The authors commented that there was currently an emphasis on fever and respiratory symptoms as criteria for suspicion of COVID-19, yet less than half the children in this analysis had those symptoms.
“Since many are asymptomatic or mild cases, children certainly are not tested as often as adults, leading to an underestimate of the true numbers of infected people and increased transmission of the virus,” they wrote.
Around one in ten patients had nasal symptoms, 8% had diarrhoea, 7% had nausea or vomiting and nearly 13% had reduced lymphocyte count.
The low rate of lymphopaenia in children was another point of difference from adults, the authors wrote, with some suggesting lymphopaenia is a predictor of prognosis in adult cases.
“With this, lymphopenia may not be a reliable indicator of COVID-19 in children,” they wrote.
TMR‘s Penny Durham asked Australian experts about some of SARS-CoV-2’s odder features, including the age breakdown, which you can read here.
10.30am, 15 April
- To speed up COVID-19 testing results for healthcare workers and frontline workers, the Victorian health department says testing specimens from healthcare personnel should be marked ‘URGENT – Health Care Worker’. If the person is being tested for return-to-work in health care or aged care, the specimen should be marked with ‘URGENT: HCW CLEARANCE TESTING, please notify result to DHHS’ and results should be copied to the DHHS COVID-19 Response and the person’s treating physician.
10am, 15 April
- TMR‘s Felicity Nelson has graphed daily new COVID-19 infections over time around Australia, which gives us this very encouraging picture:
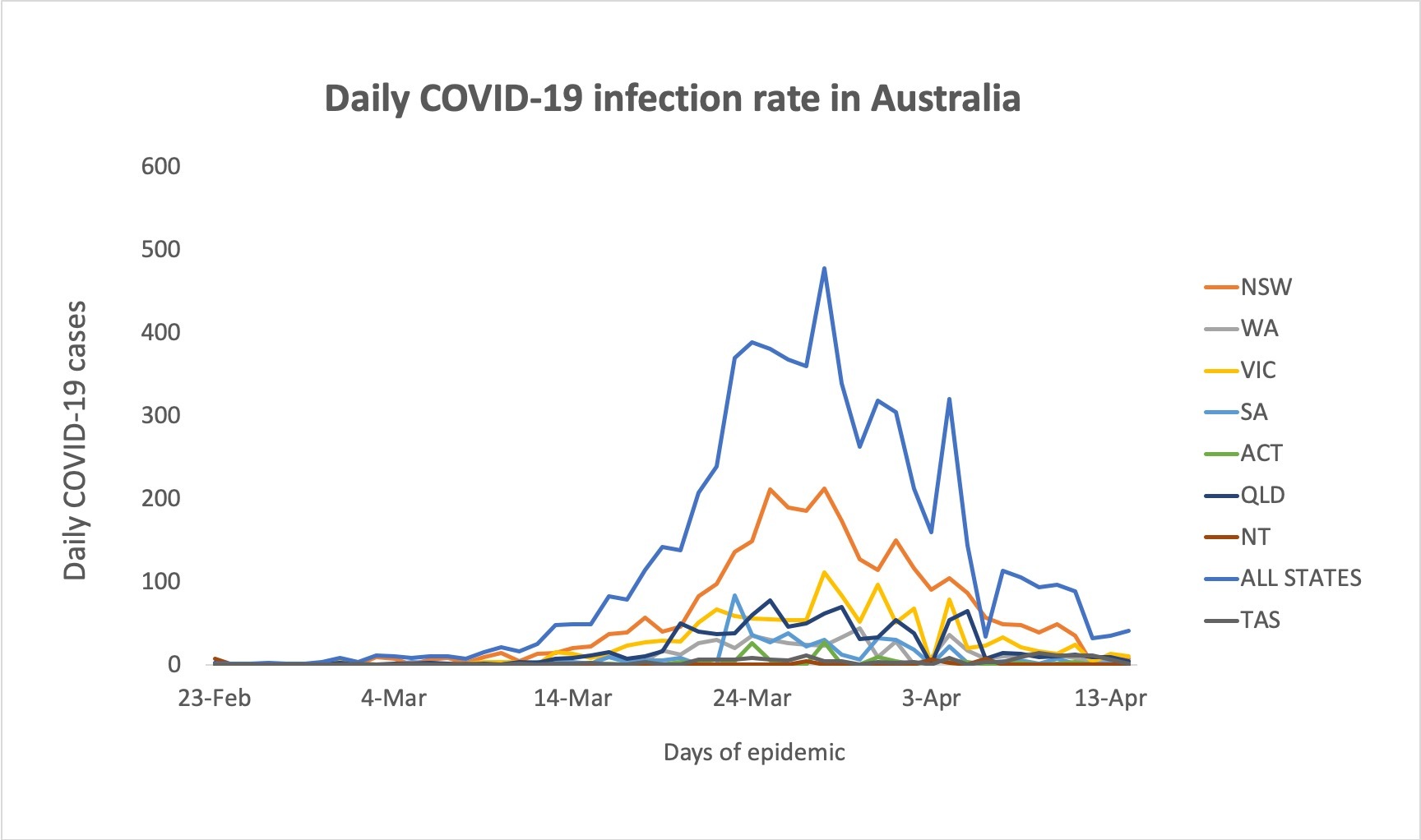
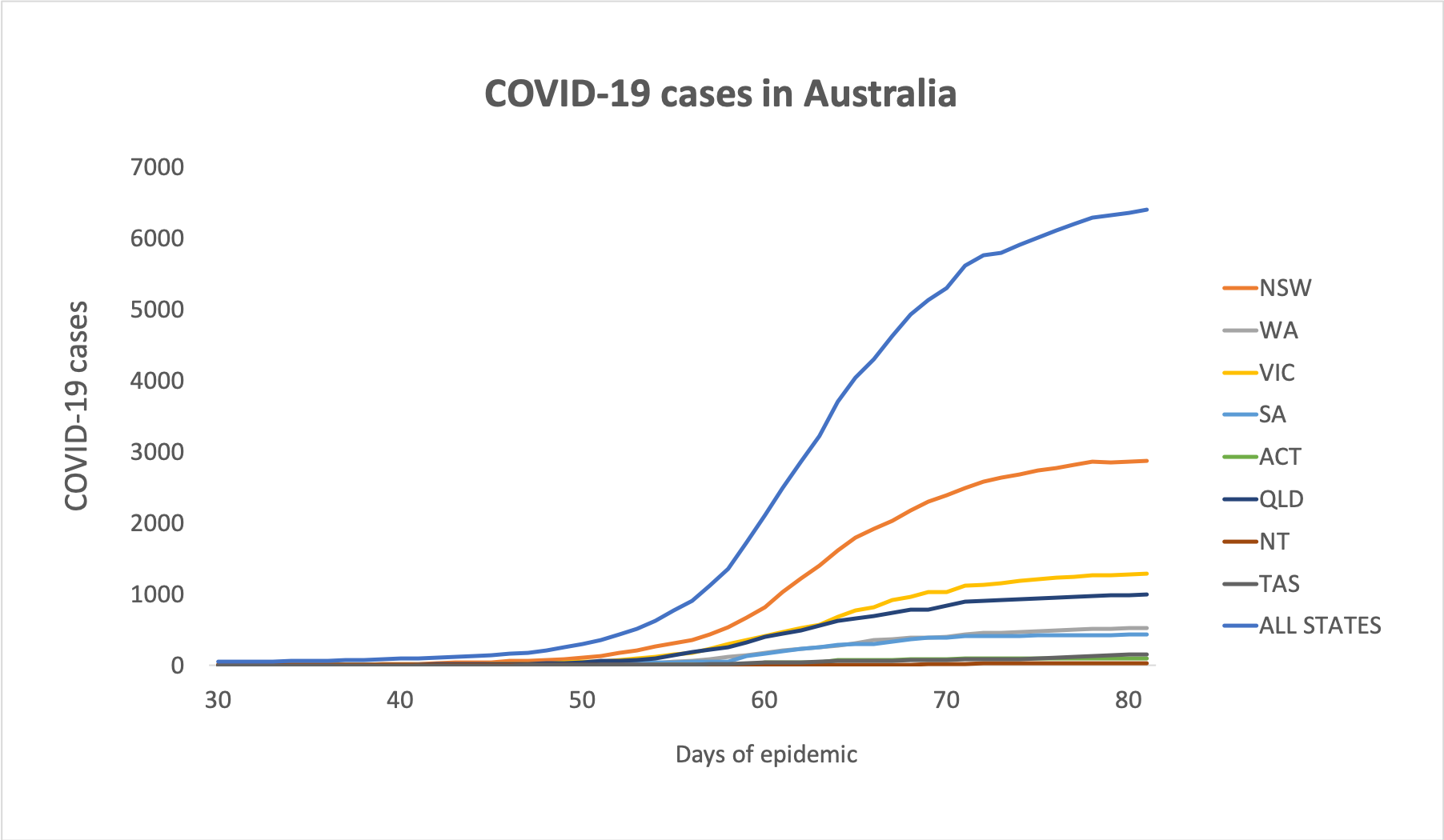
- Here are the latest figures on confirmed COVID-19 cases around Australia to 3pm yesterday:
National – 6,400 (up 41) and 61 deaths
ACT – 103
NSW – 2,870
NT – 27
QLD – 998
SA – 433
TAS – 151
VIC – 1,291
WA – 527
And in chart form (how about those non-curves, eh?):
- Australian study (preprint) suggests self-collection of nose and throat swabs to test for COVID-19 could be an option and would reduce healthcare workers’ exposure to infected patients. Victoria has expanded its COVID-19 testing criteria to include anyone with fever or symptoms of acute respiratory infection that does not have an alternative diagnosis. More than one in ten pregnant women screened for COVID-19 when admitted for delivery in New York was found to be infected despite having no symptoms. Hypertension, diabetes and ischaemic heart disease are common comorbidities among patients who die from COVID-19. The International Federation of Gynecology and Obstetrics has put out interim guidance on managing COVID-19 during pregnancy, which includes advice on monitoring, delivery and breastfeeding. And some of Australia’s biggest pathology companies are pressuring GPs for rent reductions for co-located pathology labs.
Disclaimer: The content on the Medical Republic COVID-19 blog is independently created by Medical Republic without input from Boehringer Ingelheim Pty Ltd. The views, information, or opinions expressed on the Medical Republic COVID-19 blog are Medical Republic’s own and do not necessarily represent those of Boehringer Ingelheim Pty Ltd. Boehringer Ingelheim Pty Ltd is not responsible for and does not verify the accuracy of any content on the Medical Republic COVID-19 blog.