A pre-pandemic survey of junior doctors in Australia has revealed that the majority didn’t feel able to take sick leave, even when they had respiratory symptoms.
Welcome to The Medical Republic‘s COVID Catch-Up.
It’s the day’s COVID-19 news into one convenient post. Email bianca@biancanogrady.com with any tips, comments or feedback.
18 August
- Most junior doctors don’t feel supported to take sick leave, pre-pandemic study finds.
- Face-shields associated with reduction in health worker infections.
- Ivermectin being touted as COVID-19 treatment with little evidence supporting it.
- Black Dog Institute launches mental health app for healthcare workers.
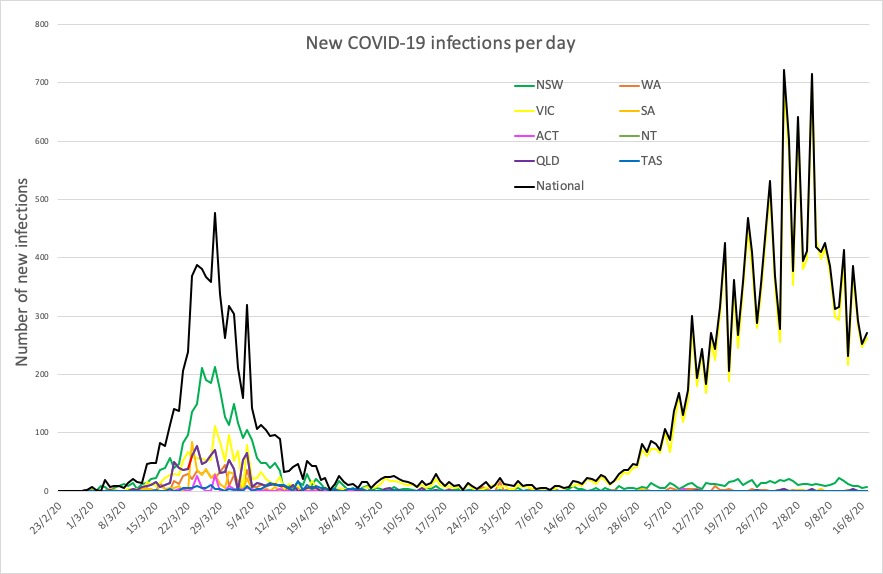
- Latest confirmed COVID-19 infection numbers around Australia.
- The phenomenon of ‘presenteeism’ – showing up to work while sick – has received much focus during the pandemic, with numerous outbreaks being attributed to individuals in a range of industries going to work despite being ill.
However a pre-COVID-19 survey of junior doctors in Canberra has revealed that the majority didn’t feel able to take sick leave, even when they had respiratory symptoms.
The survey, published in Infection, Disease and Health, surveyed 50 junior doctors in an effort to understand the barriers that prevented these healthcare workers from take sick leave when they had acute respiratory symptoms.
Researchers found that one-third of respondents had worked despite having a fever, and three-quarters of those who worked while unwell believed they were infectious.
However 86% also said they did not feel supported to take sick leave, with 96% concerned about lack of available cover and about burdening their colleagues with extra work.
“This is reflective of their experience that there is not adequate sick cover in place, that the workplace is understaffed, and that junior doctors already have high workloads,” the authors wrote.
Around half said they kept working while sick because they saw their colleagues doing the same, and half also said they didn’t take sick leave because they didn’t feel the were sick enough. Nearly half were also concerned about the impact of sick leave on their registration requirements, and just over one-third didn’t want to take leave because they had a sense of duty towards their patients and were worried that patient outcomes would be poorer if they weren’t there.
“In the era of COVID-19 there is a unique opportunity to use the heightened awareness of the implications of working whilst unwell to change the culture around presenteeism and improve the accessibility of sick leave for doctors,” the authors wrote. - A small study has found the introduction of face shields for healthcare workers was associated with a lower rate of healthcare worker infections with COVID-19.
The study, published in JAMA, looked at COVID-19 infections among 62 community health workers who counselled the families of patients who had tested positive for SARS-CoV-2.
The workers were using PPE, practising physical distancing and hand hygiene, as well as remaining isolated from family, friends and the general public. Before the introduction of face shields, there were 12 infections among the health workers, but no further cases were recorded after the workers began using face shields in addition to their other PPE.
“The face shields may have reduced ocular exposure or contamination of masks or hands or may have diverted movement of air around the face,” the authors wrote. - Ivermectin is shaping up as the new hydroxychloroquine, with some individuals – and even nations – stepping up to tout it as the new COVID-19 cure based on flimsy evidence, according to a story in newsGP.
The product, which most would know as an anti-parasitic agent and sheep drench, was tested by Australian researchers in a pre-clinical trial and shown to have antiviral action against SARS-CoV-2. But there are very few clinical trials; one study in 116 patients used a combination of ivermectin and doxycycline compared to hydroxychloroquine + azithromycin, and found no significant difference between the two groups. The best that could be said of the combination was that it was safe.
Back in April, the FDA issued a warning against using animal ivermectin in humans. There are other trials underway, but no results as yet.
But that hasn’t stopped a Sydney gastroenterologist from recently giving the product a plug on national television as a potential COVID-19 cure. - The Black Dog Institute has launched its mental health app for healthcare workers, which provides tailored advice, triage and support for those on the frontline of the COVID-19 pandemic.
The Essential Network was developed in partnership with several organisations and with funding from the Federal Government. Healthcare workers can access resources and tools, online programs, and one-on-one consultations. - Here are the latest confirmed COVID-19 infection numbers around Australia, to 9pm Monday:
National – 23,559, with 421 deaths and 674 hospitalised.
ACT – 113 (0)
NSW – 3957 (7)
NT – 33 (0)
QLD – 1091 (0)
SA – 462 (1)
TAS – 230 (0)
VIC – 17,027 (282)
WA – 646 (0)