Fauci, who was anaesthetised for surgery when the decision was made, says the new recommendations may give a false impression about the importance of asymptomatic spread.
Welcome to The Medical Republic‘s COVID Catch-Up.
It’s the day’s COVID-19 news into one convenient post. Email bianca@biancanogrady.com with any tips, comments or feedback.
28 August
- US CDC revises testing guidelines to exclude asymptomatic contacts, while Dr Anthony Fauci is under anaesthetic for surgery.
- New flowchart offers guidance on caring for elderly and frail with COVID-19
- COVID-19 and nosocomial multidrug-resistant candidiasis an emerging issue in India.
- Boston biotech conference may have resulted in tens of thousands of COVID-19 infections, researchers suggest.
- COVID-19 case fatality rate much lower in children than general population.
- Latest confirmed COVID-19 infection numbers around Australia.
- The US Centers for Disease Control found itself in public health hot water again this week after it published new COVID-19 testing guidelines that say people who have been in close contact with a COVID-19 case do not need to get tested if they don’t show symptoms. Then it turns out the White House Coronavirus Task Force member Dr. Anthony Fauci was undergoing surgery and under anaesthetic when the meeting took place to decide the new advice.
Fauci told CNN that he was concerned the new recommendations would give the incorrect impression that asymptomatic spread was not of concern, when in fact it is. - Australia’s National COVID-19 Clinical Evidence Taskforce has published a new flowchart with guidance on managing older and frail patients with COVID-19. The guidance covers subjects such as the goals of care, communication, polypharmacy, and management of delirium and anxiety.
The latest taskforce update also advises using prone positioning for at least three hours a day in adults with COVID-19 and respiratory symptoms who are receiving any form of non-invasive supplemental oxygen therapy.
For adults with COVID-19 and respiratory symptoms who are receiving any form of supplemental oxygen therapy and have not yet been intubated, consider prone positioning for at least 3 hours per day as tolerated. When positioning a patient in prone, ensure it is used with caution and accompanied by close monitoring of the patient. Use of prone positioning should not delay endotracheal intubation and mechanical ventilation in patients with COVID-19 who are deteriorating despite optimised less invasive respiratory therapies. - Clinicians in India are fighting the COVID-19 battle on two deadly fronts, as nosocomial infections with multi-drug resistant Candida auris claim the lives of patients critically ill with COVID-19.
A study published in Emerging Infectious Diseases found 2.5% of 596 patients admitted to intensive care with COVID-19 during April-July 2020 had candidiasis. Two-thirds of those patients were infected with C. auris, and 60% of this group died.
All of those patients infected with C. auris had isolates that were resistant to fluconazole, 30% were resistant to both fluconazole and voriconazole, and 30% were resistant to azoles, amphotericin B and 5-flucytosine.
The authors commented that the patients were probably infected with Candida while hospitalised, and as the COVID-19 pandemic increases the number of patients in prolonged intensive care, these nosocomial infections are of significant concern. - A single biotech conference in Boston may have been a super-spreading event that led to tens of thousands of cases of COVID-19, according to a story in The Scientist.
A study, published on the non-peer-reviewed preprint server MedRxiv, conducted phylogenetic analysis of nasopharyngeal samples collected from January-May in Massachusetts and identified 772 complete SARS-CoV-2 genomes. These included genomes from 28 cases associated with the Biogen conference in Boston in late February, which was itself associated with more than 90 cases.
A particular genetic variant that made its first appearance in the US in attendees of that Boston conference subsequent spread widely across Boston, the US, and other countries, and was identified in more than 1000 samples collected globally.
However in an interview with The Scientist magazine, one of the researchers involved with the study said they estimated that tally of infections that could be traced back to that Boston conference was likely to be more than 20,000. - The fatality rate from COVID-19 is significantly lower in children than in the general population, according to a study published in the BMJ.
A prospective study of 651 children aged under 19 years admitted to 138 UK hospitals with confirmed SARS-CoV-2 between January and July 2020 found the overall in-hospital case fatality rate was just 1%, compared to 27% for the entire age cohort across the same period. All the deaths occurred in individuals with profound comorbidities; three were neonates with severe comorbidities, two were aged 15-18 with neurodisabilities and pre-existing respiratory issues, and one was undergoing chemotherapy and had bacterial sepsis.
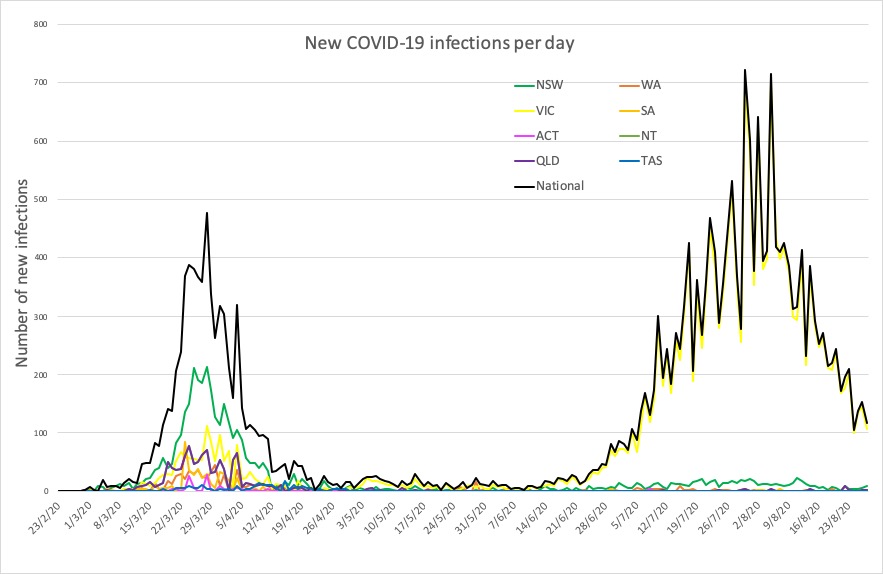
Overall, 18% of the children were admitted to intensive care and 9% were put on ventilators, and 11% of 11% of 456 patients assessed met the WHO criteria for multisystem inflammatory syndrome – the condition with similar presentation to Kawasaki disease and toxic shock syndrome. - Here are today’s confirmed COVID-19 infection numbers around Australia, to 9pm Thursday:
National – 25.322, with 572 deaths
ACT – 113 (0)
NSW – 4006 (9)
NT – 33 (0)
QLD – 1110 (2)
SA – 463 (0)
TAS – 230 (0)
VIC – 18,714 (113)
WA – 653 (0)