And study finds most older Australians have at least one risk factor for COVID-19.
Welcome to The Medical Republic’s COVID Catch-Up.
It’s the day’s COVID-19 news in one convenient post. Email bianca@biancanogrady.com with any tips, comments or feedback.
2 February
- Warning against mistaking COVID-19 symptoms for post-vaccine side effects.
- Half of Australia’s elderly have two or more risk factors for COVID-19.
- Shock associated with more serious illness in paediatric multisystem inflammatory syndrome associated with COVID-19.
- Latest confirmed COVID-19 infection numbers from around Australia.
Researchers have warned against dismissing COVID-19 symptoms as post-vaccination side effects, after a study found a number of vaccinated healthcare workers in Israel developed COVID-19 in the few days after receiving their first vaccine dose.
The study, published in Emerging Infectious Diseases, described the follow-up of 4,081 healthcare workers who were vaccinated with the Pfizer-BioNTech vaccine in the first week of the vaccine roll-out, at a time when Israel’s COVID-19 infection rate rose above 6%.
Following the first vaccine dose, 22 healthcare workers tested positive for SARS-CoV-2, 13 of whom had developed symptoms including fever, chills, cough, headache and myalgia.
Noting that the vaccine in question is not thought to offer complete protection in the first few days after the first dose, the study’s authors urged caution in overlooking potential COVID-19 symptoms.
“Clinicians should have a high level of suspicion of reported symptoms and avoid dismissing complaints as vaccine-related until true infection is ruled out and vaccinees are tested,” they wrote. “Active and passive surveillance schemes that enable rapid testing and initiation of infection control measures are essential in preventing possible diagnostic delays and secondary exposures.”
Nearly 80% of older Australians have at least one risk factor for poorer COVID-19 outcomes, and this is even more so among those in residential care, a study has found.
Writing in the Australian Journal of General Practice, researchers present the findings of a study of health claims data for more than 103,000 Department of Veterans’ Affairs clients, around 90% of whom were living in the community.
The most common single risk factor was cardiovascular disease, which was present in 38.5% of community-dwelling individuals and 36% of those in aged care.
However more than half of the entire cohort had at least two risk factors – most commonly cardiovascular disease combined with either respiratory, diabetes or immune risk factors – and one in five had three or more risk factors.
Around 40% of children who develop multisystem inflammatory syndrome associated with COVID-19 present with shock, and these tend to have a higher rate of gastrointestinal, cardiorespiratory, and neurologic symptoms, according to new research.
A paper published in Pediatrics describes the clinical features and outcomes of 183 paediatric cases of the COVID-19-associated illness, from 33 hospitals across Europe, Asia and the Americas.
Researchers identified three types of presentation among the syndrome. Around 42% presented with shock, and these tended to have significantly lower platelet count and higher levels of NT-proB-type Natriuretic Peptide, D-dimer, C-reactive protein, and ferritin.
Another 42% presented with what the authors described as incomplete Kawasaki disease presentation, which included gastrointestinal and respiratory symptoms.
The third group, which was nearly 15% of patients, presented with Kawasaki-like disease symptoms such as mucocutaneous involvement, lymphadenopathy and conjunctivitis.
The Kawasaki-like disease group had significantly better outcomes over all compared to the other two groups. Those with shock had significantly longer hospital stays and were more likely to be admitted to intensive care and require mechanical ventilation compared to those with Kawasaki-like disease or incomplete Kawasaki-like illness.
A shorter time between symptoms and admission to hospital was also associated with worse outcomes.
Overall, 30% of the group were Black, nearly 60% were male and just over one-quarter were obese. While 86% had positive serological test results for SARS-CoV-2 exposure, only 37% tested positive on RT-PCR, and fewer than two-thirds had evidence of current or recent COVID-19.
Nearly 40% were treated with IV inotropic medication, 23% needed mechanical ventilation, and four patients were treated with extracorporeal membrane oxygenation. Three died, all aged under three years.
West Australia’s health department has released a list of locations around Perth, Nedlands, Maylands and several other areas that were visited by the quarantine hotel security guard who has since tested positive for COVID-19. Anyone who visited those locations is asked to get tested for SARS-CoV-2 and remain in quarantine until they receive a negative result.
No other infections have been reported in association with that one case.
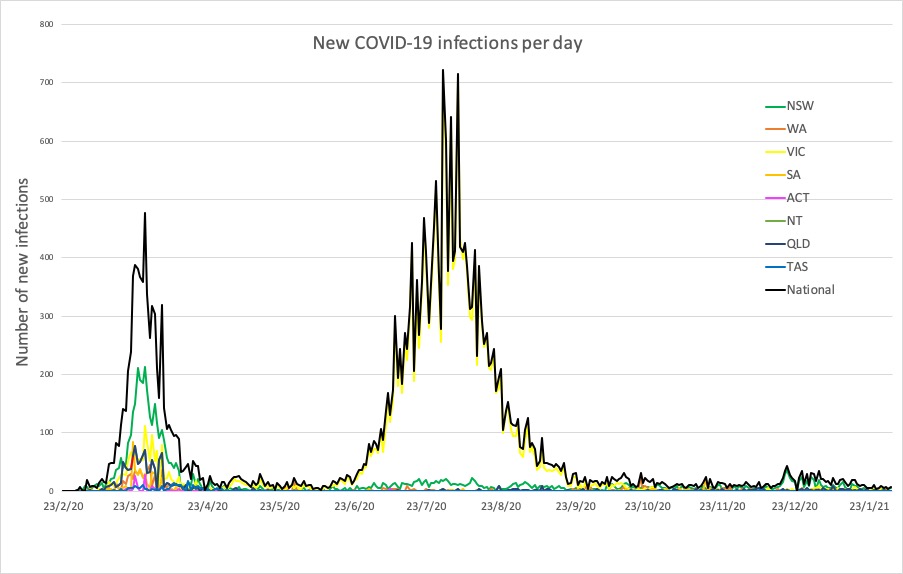
Here are the latest confirmed COVID-19 infection numbers from around Australia to 9pm Monday:
National – 28,818 with 909 deaths
ACT- 118 (0)
NSW – 5110 (6)
NT – 98 (0)
QLD – 1310 (0)
SA – 596 (0)
TAS – 234 (0)
VIC – 20,449 (1)
WA – 903 (1)