A free 24-hour online mental health support service has been set up by Beyond Blue to help Australians deal with the psychological challenges of the COVID-19 pandemic
That’s it for this (short) week on The Medical Republic‘s live COVID-19 blog.
Thanks to our sponsor and supporter for funding this project with an independent grant, Boehringer Ingelheim.
Have a safe, relaxing and healthy long weekend.
The latest
- The AMA drops a new COVID-19 fact file, this one on pharmacologic therapies.
- Free 24/7 mental health support now available online and by phone from Beyond Blue.
- Some guidance for GPs on managing opioid-dependent patients during the pandemic.
5.10pm, 9 April
- The AMA has released its second evidence-based fact file, this one on the many pharmacologic therapies being investigated (or just touted) as possible COVID-19 treatments.
AMA Federal Vice President Dr Chris Zappala looks at everything from convalescent plasma and nucleoside analogues to the famed hydroxychloroquine and novel antiviral agents.
- A free 24-hour online mental health support service has been set up by Beyond Blue to help Australians deal with the psychological challenges of the COVID-19 pandemic.
The service, which is backed by funding from the Australian government, includes a 24/7 hotline number staffed by mental health professionals, an online community forum, information and advice, and a crisis support service.
There is also information tailored to small businesses owners, to those who have small children, the unemployed and healthcare professionals.
2.50pm, 9 April
- Dog people rejoice; it seems that SARS-Cov-2 replicates poorly in canines. Cat people; I’m afraid your furry feline is at risk.
That’s the word according to Science, which has just published a study suggesting that ferrets and cats are able to be infected with SARS-CoV-2, but dogs, pigs, chickens and ducks don’t seem to be as susceptible.
The experiments, which were performed in high biosafety level facilities in China, also suggest that cats are susceptible to airborne infection, which might explain how a tiger in the Bronx Zoo was diagnosed with the disease recently (and that’s a whole other Netflix series).
- If you have patients undergoing treatment for opioid dependence, there are now specific guidelines available to help GPs manage these patients during the COVID-19 pandemic.
The guidelines, which have been put together by a working group including experts from the RACGP, the Pharmacy Guild and the Victorian Alcohol and Drug Association, suggest taking steps such as:
– giving scripts up to six months duration, in case you become unwell;
– consider giving stable patients up to 1 month of Suboxone or up to 1-2 weeks of methadone, after conducting a risk assessment;
– move patients to long-acting buprenorphine where possible and if you are able to prescribe and administer;
– solo practitioners should try to find a buddy or delegate who can cover them if they become unwell;
– give all patients scripts for take-home naloxone and educational material on overdose identification, first aid and naloxone administration.
11.55am, 9 April
- It turns out alcohol-based hand sanitisers and naked flame are a bad combination. NSW fire authorities have put out a reminder to anyone planning to BBQ in these times that they should make sure their hand sanitiser has completely dried before lighting up, in order to avoid flame-grilling their lovely virus-free hands.
- Around one in ten children with confirmed COVID-19 infection were admitted to paediatric intensive care in Madrid, according to new data.
A research letter published in JAMA Pediatrics reports a case series of 365 children with potential COVID-19 symptoms who were tested at 30 hospitals in Madrid over two weeks; 41 (11.2%) of whom were positive.
Sixty percent of those diagnosed with COVID-19 were hospitalised, four were admitted to ICU and needed more high-flow respiratory support – one of whom had pre-existing recurrent wheezing.
However the authors stressed that testing for infection in these hospitals was initially only done on patients with symptoms, comorbidities, and at high risk of complications, so their results may be biased towards moderate to severe cases.
Around one-third of those who tested positive had upper respiratory tract infection symptoms, one-quarter had fever, 15% had viral-like pneumonia, and two of them had gastroenteritis or vomiting.
Overall in the Madrid region, 0.8% of the 4695 confirmed cases of COVID-19 diagnosed by March 16 were in children aged under 18 years.
Another report from the US Centers for Disease Control, published on April 6 in Morbidity and Mortality Weekly Report, found that 1.7% of the nearly 150,000 cases of COVID-19 that occurred from February to April were in those aged under 18. This data showed that only three-quarters of paediatric cases had symptoms of fever, cough or shortness of breath, compared to 93% of adults.
10.50am, 9 April
- The Guardian newspaper has highlighted the plight of cash-strapped GPs, saying that small medical practices are on the brink of collapse.
The story, which also reported The Medical Republic’s survey of GPs showing around half had lost at least 30% of their revenue, also quoted AGPA saying that the primary healthcare system in Australia relied on these small businesses.
A Brisbane GP interviewed in the story said she and her business partner had stopped paying themselves an income after their bookings dropped 50% and the clinic was forced to bulk-bill the majority of its patients.
10.20am, 9 April
- From TMR’s Penny Durham: If your practice isn’t yet set up for telehealth, or you’re struggling with it, don’t get left behind – help is available.
With 2.5 million consultations since Medicare rebates were introduced, telehealth is becoming the new normal; but that doesn’t mean the transition is instant or easy.
The Digital Health CRC is running a webinar tonight at 6pm AEST to help you choose tools and technology, redesign your workflow, and engage with staff and patients. It’s hosted by two GPs highly experienced in telemedicine: Bondi-based Dr Amandeep Hasra, former chief medical officer for Telstra Health and senior medical adviser at Medibank Health Solutions, among other things; and Dr David Triska, who runs a digital-first practice in Surrey, UK. More information and registration here: https://www.digitalhealthcrc.com/telehealth-implementation/
- TMR’s Penny Durham reports: The Medical Journal of Australia has released a preprint on the clinical presentation, assessment and management of COVID-19.
Led by Dr Irani Thevarajan, an infectious diseases clinician at Royal Melbourne Hospital, the paper outlines how to assess whether a patient can be managed in the community or requires admission.
It also reviews the evidence for a range of proposed drug therapies, noting that “No good clinical evidence for any specific therapies (including antiviral and immune modulating agents) currently exists.”
The authors conclude: “Biomedical innovations such as new and rapid point-of-care diagnostics, effective specific treatments, and preventive vaccines are very high priorities … In the interim, high quality, evidence-based clinical care – scaled up to face the pandemic challenge – will save the lives of thousands in Australia, and
millions globally.”
Some other fast facts from the paper:
– COVID-19 has an estimated median incubation period of 5.1 days, and 97.5% of patients who develop symptoms will do so within 11 days of exposure (hence the 14-day quarantine period)
– Fever has been reported in 99% of patients at some period during their illness, but is only reported in 44% of patients at the time of hospital admission.
– COVID-19 infection presents as a mild respiratory illness in four out of five ambulatory patients. Around 15% need hospital care, and another 5% need intensive support.
– Shortness of breath, lower initial oxygen levels, higher serum white blood cell count and lower lymphocyte count are all more common in patients who die from COVID-19 than those who survive.
– Patients with mild disease can be managed in the community as long as they are able to monitor their condition and know when to go to hospital.
- What did you miss yesterday? The big news was the government’s announcement that 11 million face masks are winging their way to Australian healthcare workers – including 1.5 million for GPs – and you all got praised as ‘heroes’ by Federal Health Minister Greg Hunt. There have been 2.5 million telehealth consultations since the introduction of the telehealth program, and the RACGP reminded everyone that telehealth also includes telephones. But it’s still not enough because GPs are struggling and need a rescue package, says the Australian General Practice Alliance. Professor Michael Kidd and Dr Tony Barton reminded Australians to look after their non-COVID-19 health issues.
- Here are the latest infection figures from around Australia, to 3pm yesterday:
National – 6,013 confirmed cases (up 105) and 50 deaths
ACT – 99
NSW – 2734
NT – 27
QLD – 943
SA – 420
TAS – 97
VIC – 1212
WA – 481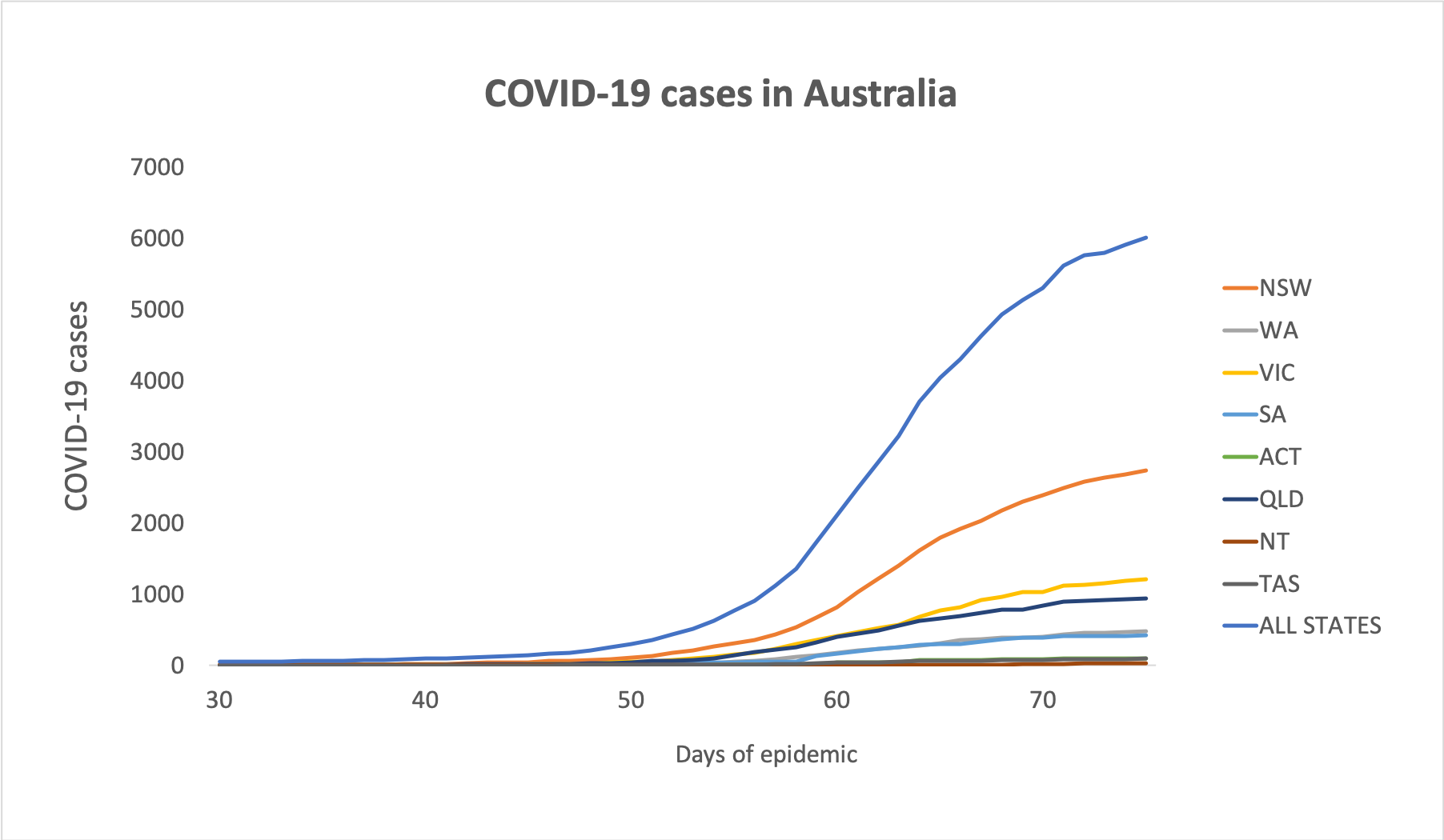
Disclaimer: The content on the Medical Republic COVID-19 blog is independently created by Medical Republic without input from Boehringer Ingelheim Pty Ltd. The views, information, or opinions expressed on the Medical Republic COVID-19 blog are Medical Republic’s own and do not necessarily represent those of Boehringer Ingelheim Pty Ltd. Boehringer Ingelheim Pty Ltd is not responsible for and does not verify the accuracy of any content on the Medical Republic COVID-19 blog.


