Triggers that may predispose to episodes of SVT include medications, drinking large amounts of caffeine or alcohol, stress and smoking
Triggers that may predispose to episodes of SVT include medications (asthma inhalers, cold remedies), drinking large amounts of caffeine or alcohol, stress or emotional upset, and smoking.
INTERVENTION
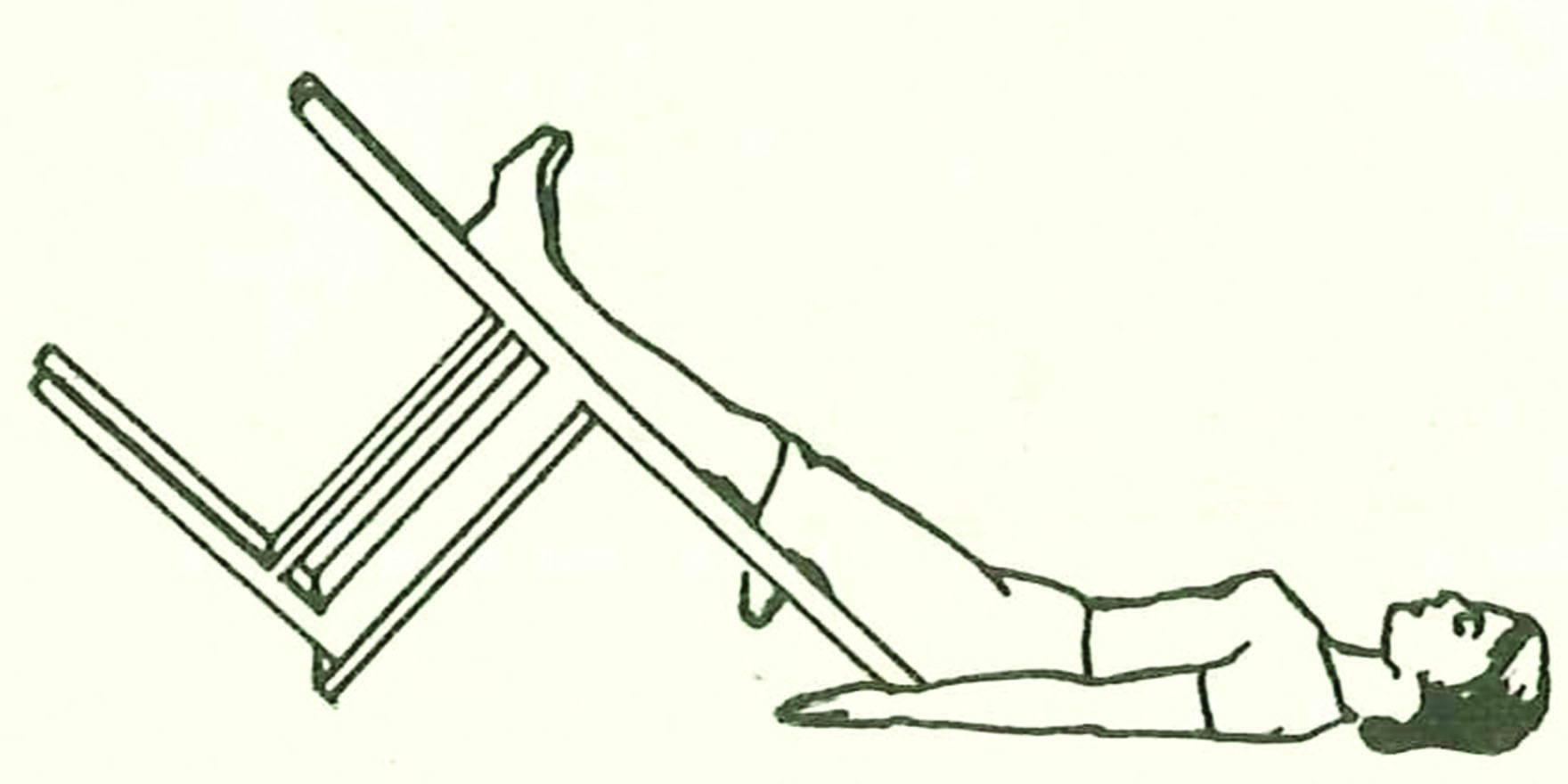
Modified Valsalva manoeuvre with passive leg elevation and supine positioning at the end of the strain.
The Valsalva manoeuvre increases vagal tone, slows conduction through the atrioventricular (AV) node and prolongs the AV nodal refractory period, leading to a reduction in heart rate and reversion of supraventricular tachycardia.
INDICATION
Supraventricular tachycardia. (SVT)
SVT refers to a variety of tachyarrhythmias that originate from atrial or AV nodal tissue including atrioventricular nodal re-entrant tachycardia (AVNRT) and atrial tachycardia, which is more common in patients with Wolff-Parkinson-White (WPW) syndrome.
Episodes of SVT may last seconds, minutes or hours. Symptoms may include awareness of tachycardia, palpitation, dizziness, breathlessness, mild chest discomfort and syncope, although some patients remain asymptomatic.
The standard Valsalva manoeuvre is recommended internationally as one of several treatment options for patients with SVT. In clinical practice, however, it terminates SVT in only 5 to 20% of cases.
In the largest randomised trial of vagal manoeuvres for the treatment of SVT, the modified Valsalva was shown to revert 43% of participants with SVT to sinus rhythm at one minute, with a number needed to treat (NNT) of four to restore sinus rhythm in one patient.
This trial did not identify any adverse events associated with the modified Valsalva manoeuvre technique.
CONTRAINDICATIONS
Valsalva manoeuvres are contraindicated in patients with SVT associated with:
• acute myocardial infarction
• haemodynamic instability (eg systolic blood pressure <90 mmHg)
• aortic stenosis
• carotid artery stenosis
• glaucoma or retinopathy
PRECAUTIONS AND ADVERSE EFFECTS
Acute myocardial infarction should be considered and excluded, especially in “at risk” patients experiencing their first episode of SVT.
Interventions that increase vagal tone can result in adverse events, including sinus pauses, AV block and syncope.
AVAILABILITY
The modified Valsalva can be performed in any location, as long as the patient can safely undertake a Valsalva strain and be repositioned. Patients with, or at risk of, recurrent SVT can be taught how to perform the technique for themselves.
DESCRIPTION
The patient is placed in a semi-recumbent position and instructed to exhale forcefully (strain) into a manometer to generate a pressure of 40 mmHg for 15 seconds. This is followed by supine repositioning and passive leg raising to 45 degrees for 15 seconds. The patient is then returned to the semi-recumbent position for a further 45 seconds before re-assessment of cardiac rhythm. (Also see Training.)
Where a manometer is not available, a 10-mL syringe blown to just move the plunger generates a similar pressure.
Blood pressure, electrocardiogram (ECG) and heart rate should be monitored during the manoeuvre. The expected response has four phases:
• Phase one – a transient increase in aortic pressure and a compensatory decrease in heart rate, due to increased intrathoracic pressure generated during forced exhalation against resistance.
• Phase two – the end of the transient period, with a decrease in aortic pressure as a consequence of reduced venous return and hence cardiac output, with baroreceptor response leading to increased heart rate.
• Phase three – the end of the strain phase of the Valsalva manoeuvre, with further decrease in aortic pressure and compensatory rise in heart rate.
• Phase four – increased venous return accentuated by raising legs leading to increasing aortic pressure and compensatory decrease in heart rate, with subsequent return to resting heart rate.
TIPS AND CHALLENGES
Although the Appelboam et al. (2015) study was conducted in hospital emergency department settings, there is no reason to assume that the modified Valsalva manoeuvre would not be both effective and safe for SVT reversion in general practice settings, as long as precautions are taken (see Contraindications and Precautions).
For patients who do not revert to sinus rhythm with the modified Valsalva manoeuvre, vagal tone can be increased by other techniques, including carotid sinus massage (CSM).
Carotid sinus massage is less effective than the Valsava manoeuvre and has around 1% risk of neurological complications, although these are usually transient. In addition to the same cardiovascular contraindications and precautions as for the modified Valsava manoeuvre, CSM is contraindicated in patients with carotid bruits or recent transient ischaemic attack (TIA) or stroke. As with the modified Valsalva manoeuvre, electrocardiogram (ECG) and heart rate should be monitored.
To perform CSM, the patient is placed in the supine position. Either the right or the left carotid sinus is gently massaged for at least five but no longer than 10 seconds, with care to avoid carotid artery trauma or occlusion. (The carotid sinus is located inferior to the angle of the mandible at the level of the thyroid cartilage, at the site of the arterial impulse.) If there is no reversion, CSM can be performed on the other side, after a one to two minute delay.
Grading: NHMRC Level II evidence.
Consumer resources:
Patient.info provides information about supraventricular tachycardia
References:
1. Appelboam A, Reuben A, Mann C, et al. Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): A randomised controlled trial. Lancet 2015;386(10005):1747–53.
2. Collins NA, Higgins GL. Reconsidering the effectiveness and safety of carotid sinus massage as a therapeutic intervention in patients with supraventricular tachycardia. Am J Emerg Med 2015;33:807–9.
3. Smith G. Management of supraventricular tachycardia using the Valsalva manoeuvre: A historical review and summary of the published evidence. Eur J Emerg Med 2012;19(6);346–52.
© The Royal Australian College of General Practitioners. First published April 2016 in the RACGP’s Handbook of Non-drug Interventions