Added support for primary care health workers would make the national disability insurer more efficient and targeted, the RACGP says.
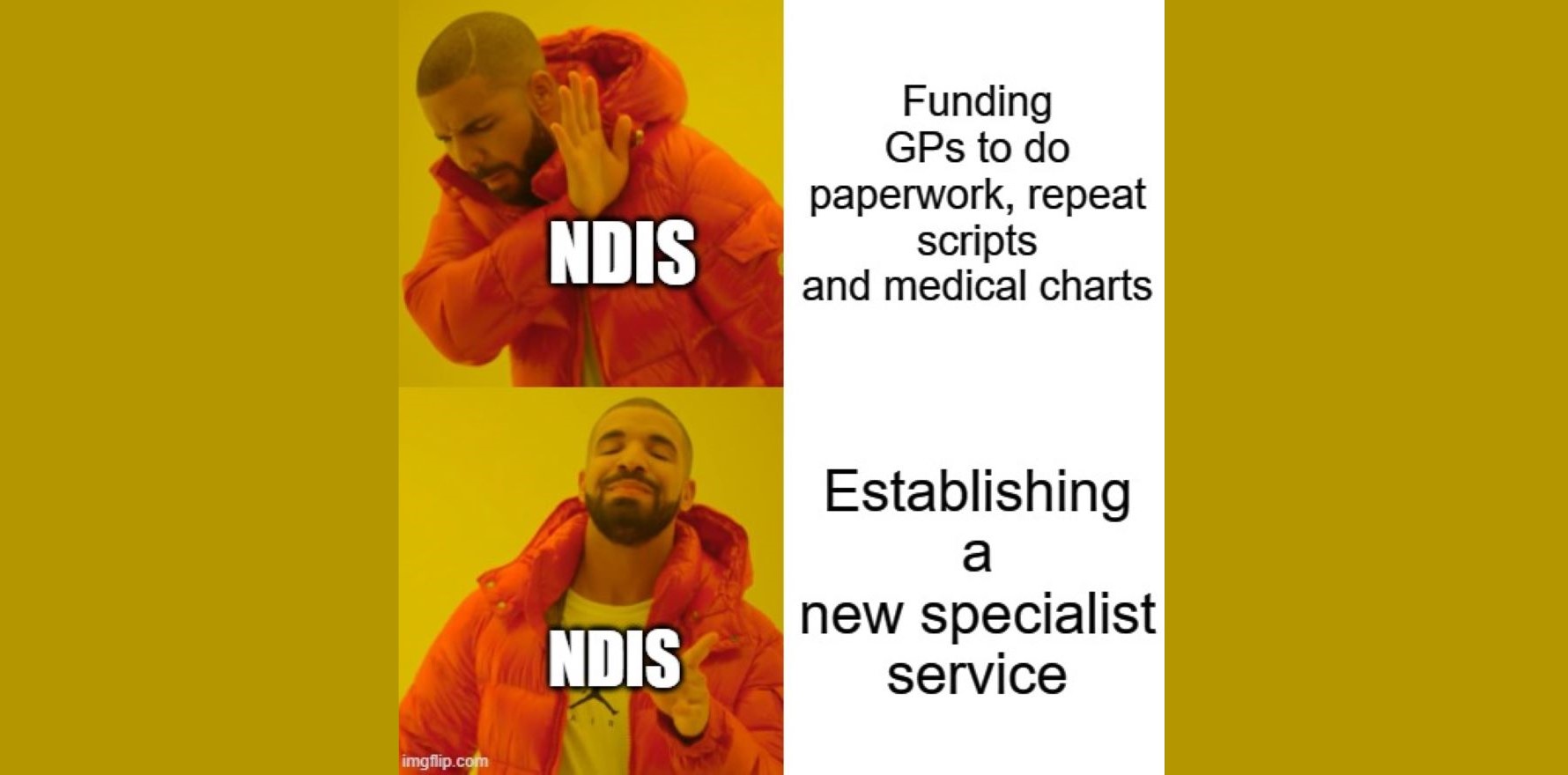
The NDIS should put money toward making the system friendlier to GPs and other primary healthcare clinicians before introducing new specialised services, according to the RACGP.
In a new submission to the Royal Commission into violence, abuse, neglect and exploitation of people with disability, the RACGP took the commissioners to task for seemingly excluding general practice from a recommendation that states establish specialised health and mental health services for people with cognitive disability.
These services would provide specialist assessment, preventative care and clinical services for people with cognitive disability and chronic health needs, as well as training for clinicians.
“The RACGP notes that there is no mention of general practice or primary care and therefore the recommendation fails to address the key role played by GPs in disability and support,” the college submission read.
Under the current settings, it continued, GPs are disincentivised to take on patients with a disability. The MBS favours shorter consults, the paperwork requirements for the NDIS are notoriously time-consuming and tasks like writing repeat prescriptions and updating charts are only remunerated if the patient is physically sitting in the clinic with the GP.
“GPs can make NDIS planning more efficient, reduce duplication, and better target supports because they know their patient and what works for them,” college president Dr Nicole Higgins said.
“As it stands, patients’ Medicare rebates don’t cover the true cost of providing comprehensive care to people with disability, and GPs are often left out of pocket for things, like completing NDIS paperwork if the patient isn’t present.
Related
“Rather than funding the establishment of new services for people living with cognitive disability, the smartest and most-cost effective investment would be to fund multi-disciplinary care teams with GPs.
“We shouldn’t reinvent the wheel, it’s costly and causes fragmentation of care which isn’t good for a patients’ health.”
In response to a recommendation to introduce dedicated disability health navigators, the RACGP again noted the “key role” that GPs play in coordination of care for people with disability and that multidisciplinary care teams could represent “better use of limited resources”.
The remainder of the RACGP’s submission focussed on existing curriculum, CPD requirements and educational activities relating to people with disability.
Separate to the Royal Commission response, NDIS Minister Bill Shorten announced yesterday that $11.6 million would go toward the “foundational supports” strategy recommended in the independent review of the NDIS, which was also conducted last year.
These foundational supports will include “general” supports, for all people with disability, and “targeted” supports for people who are not eligible for the NDIS.
General supports include things like assistance with shopping and property maintenance, whereas targeted supports will be things like mobility aids and early support services.
These will largely be external to the NDIS.
“This strategy will address the gap between NDIS and non-NDIS systems, prioritising the need for responsive services that allow all people with disability to fully participate in their communities,” Mr Shorten said.