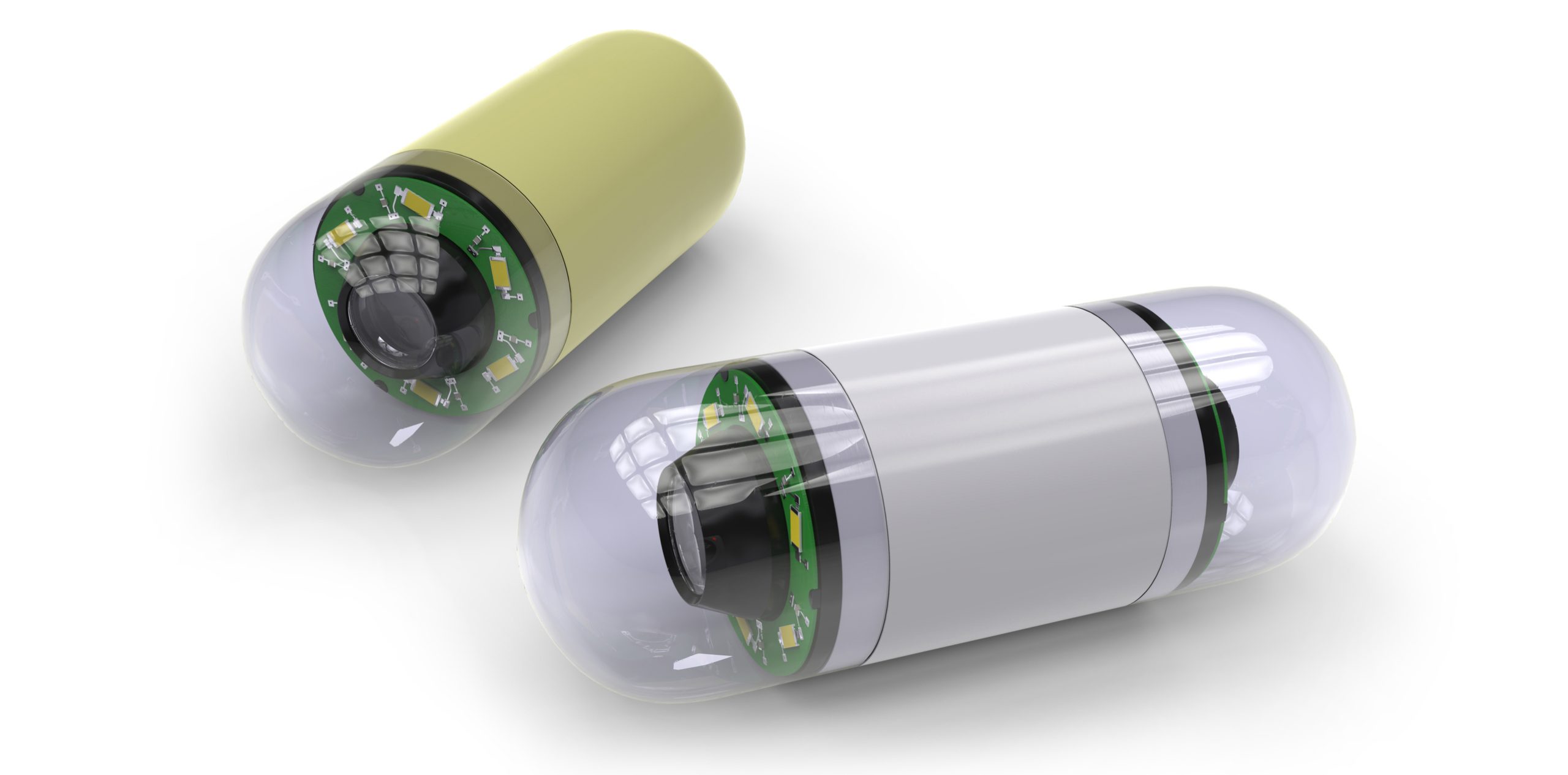
Telecare and Mackay HHS developed the service, reducing wait times and the need for patients to travel thousands of kilometres for a capsule endoscopy.
A partnership between Australian virtual health provider Telecare and the Mackay Health and Hospital Service in north Queensland has created a care pathway for patients needing capsule endoscopy, reducing wait times from as much as 1000+ days down to “very manageable”.
When a private arrangement collapsed in 2023, Mackay HHS found itself without an inflammatory bowel disease specialist service, leaving patients who needed a “pill cam” endoscopy high and dry and facing travel to either Townsville or Brisbane for the procedure.
“Luckily we had a very competent and dedicated IBD specialist clinical nurse who was able to service the patients on our IBD wait list reasonably well, but she was struggling because she didn’t have specialist support and there was no pill cam endoscopy service available,” said Cathie La Riviere, Mackay HHS’s manager of virtual care.
While the number of patients on the wait list wasn’t huge – about 20 at any one time – those patients were “frequent flyers” into Mackay Hospital’s emergency department and wards.
An IBD specialist who already worked with Mackay HHS through virtual care was accredited for pill cam reporting.
“So, the idea was born that we could use [the clinical nurse] to do the procedures in the hospital, and then we could use [the specialist] to do reporting from a remote location.”
Enter Telecare, which services over 300 virtual specialists in over 30 specialties to the tune of about 3000 consultations a month, providing virtual inpatient, virtual outpatient and remote reporting services.
Between January and October 2024, Telecare and Mackay HHS worked together to codesign a model that could smooth the path for patients needing capsule endoscopies.
“We thought we could do this pretty quickly, because everyone was onboard and thought it was a fantastic idea,” said Ms La Riviere.
Then started a lengthy period of stakeholder engagement. Agreement on treatment protocols and escalation pathways – now involving the surgical department and others – followed some negotiation and collaboration.
“Protocols and instruction manuals were developed, and that was signed off,” said Ms La Riviere.
“And then we had to purchase field cam equipment, hardware and software systems and single use devices. We had to deliver training to different staff. We created information sessions for our patients.
“We also had to complete a privacy impact assessment, and cybersecurity checks to meet our ICT requirements for privacy and security, given that we were providing access to a remote specialist.
“We also had to re-credential [the remote specialist] to include capsule endoscopy reporting as to meet our clinical governance requirements.”
Related
Once the program was able to start the pill cam wait list quickly became well managed, she said.
“We have clear referral pathways that are assisting to get the right patients access to pill cam in a timely manner and then followed up with appropriate treatments far more quickly than previously.
“Our local staff are involved in the service, and they’re learning on the job and upskilling to better manage this cohort. Having access remotely means that [the specialist] can do this from anywhere, anytime, with the potential to scale it up to our hospitals in, potentially, Bowen and Proserpine.”
Dr Ray Wen, Telecare’s chief growth officer and medical director of primary care services, said the current wait list was “more dependent on the patient’s availability than the clinicians’ availability”.
“When we first started, the longest patient on the waitlist was on the waitlist 1085 days,” he said.
“The clinical results identified included three patients with active bleeding from a total of 32 cases reviewed up to June 2025, and one potentially lifesaving – a carcinoma that was found which was not previously identified, and it prompted endoscopic confirmation in the surgical resection.
“The patient had already been referred for work-up for iron deficiency anaemia. They had a previous failed colonoscopy, and then they had a scan to replace the colonoscopy, which was reported normal.
“They had waited for about 300 days on the wait list when they were first assessed, and then, as a result of the pill cam service, the tumour [was identified], the patient was appropriately referred on, had surgical resection and likely good outcomes,” he said.
“This shows the power of in-time diagnostics, they were one of the first patients seen within this program.”
One hundred percent of the patients rated the overall experience as good or excellent and 85% of patients rated the communication and follow-up of results as good or excellent.
“These are models that everyone can implement,” said Dr Wen.
“It doesn’t have to be with Telecare, but the protocol build-out took a lot longer than was anticipated.
“There were some governance overheads, like a new procedure form that took six months of reviews to approve.
“And then there were some downstream things that maybe when we first started we hadn’t thought about, like what do we do if we find something, essentially.
“But on the back of this successful remote reporting program, my understanding is the Mackay gastroenterologists are [now] upskilled so that they can do the push enteroscopy – which is the treatment for small bowel bleeds – in house, and that will smooth the process even more so.”
There was still work to be done on educating local GPs about the availability of the service, said Dr Wen.
“And the escalation pathway piece is important for anyone who does want to implement something like this to ensure that there is an appropriate escalation pathway.”
Cathy La Riviere and Dr Ray Wen were speaking at the AIDH’s HIC2025 conference held in Melbourne on 18, 19 and 20 August 2025.