The great work GPs do often flies under the radar, but for the health of the nation, awareness needs to improve
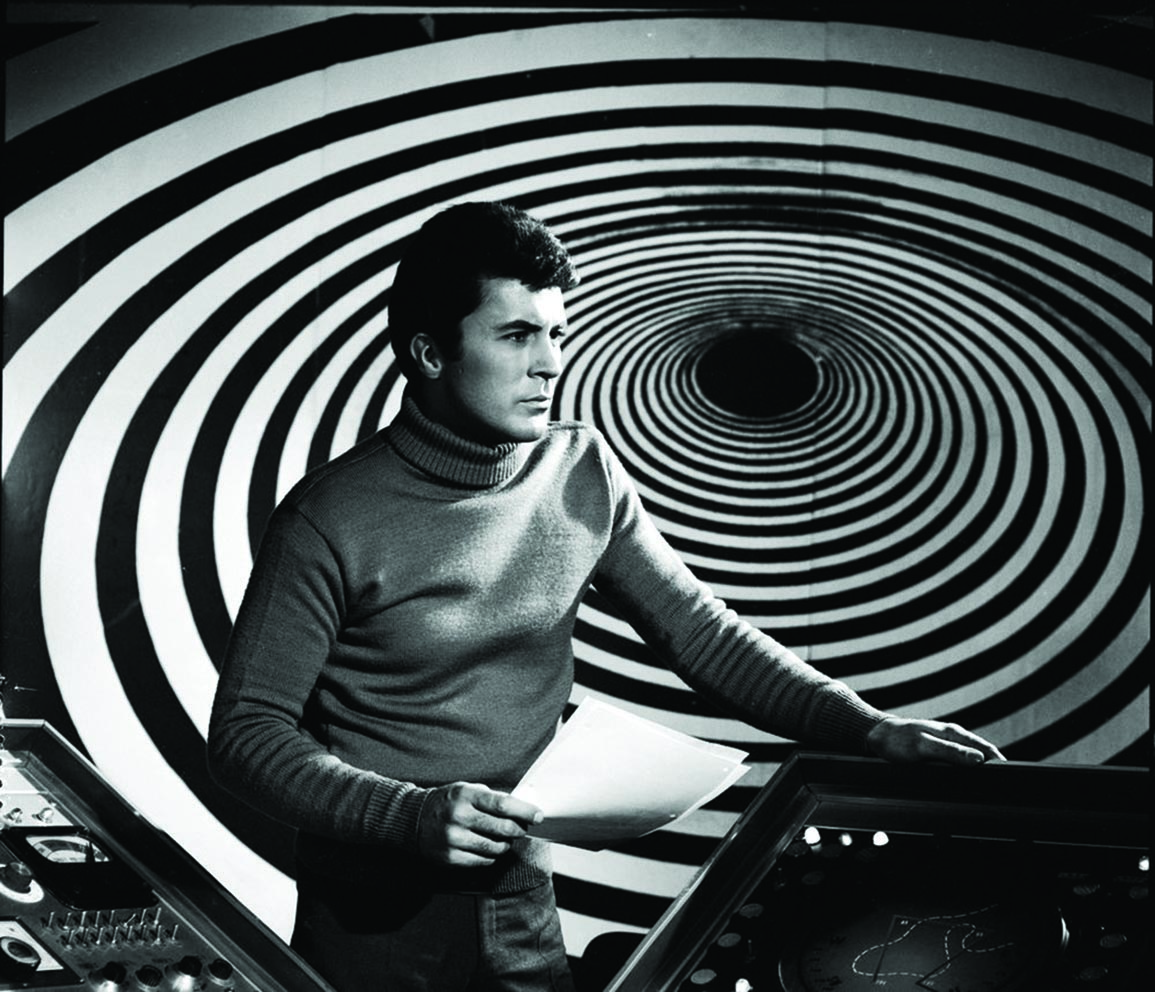
Senior lecturer and Fremantle general practitioner, Dr Brett Montgomery, likes to conduct a time-travel experiment with his third-year medical students at the University of Western Australia.
He begins by painting the picture of a person collapsing with a likely heart attack, who’s rushed to a hospital emergency department where doctors and nurses dash to his aid. He’s in VF and fortunately, defibrillation is successful. The patient slowly opens their eyes, and another life is saved. Dramatic stuff worthy of depiction in a hospital-based TV series.
It’s here that Dr Montgomery pauses and takes students back in time, to a period five years before the patient’s life-changing episode occurred.
“What if we had a time machine?” he asks.
His students are metaphorically transported back to an occasion when the same patient saw their GP.
After a thorough history and examination, the GP calculated a high risk of the patient suffering a myocardial infarct in the next five years. She prescribed antihypertensives and cholesterol-lowering medication.
Now the time machine returns the students to the day of the patient’s almost fatal arrhythmia. This time, the day passes without incident for the patient because of a decision made five years earlier, and subsequent continuous care in the GP’s hands.
“The image of the patient being saved makes for a very dramatic story,” Dr Montgomery told The Medical Republic.
“But if you knew that person was going to have an arrest and could prevent it from ever happening … in a sense, that is even more amazing and impressive.
I use this for my students to explain how general practice is so important.”
The reality, however, is that we can’t predict the future, at least not with certainty. So prescribing pills in a suburban clinic for something that has yet to happen does not set the pulse racing or fire the imagination. Hence Dr Montgomery’s time-travelling experiment.
Therein lies one of the inherent issues around the perception of primary care, as grossly unfair as it may be. General practice contains a fraction of the drama, commands fewer headlines and has none of the political currency that accompanies the “heroic” hospital and emergency intervention end of town.
In short, the work of a GP can often fly under the radar, undervalued in comparison to the more celebrated areas of the healthcare system.
“I think a lot of GPs would probably agree that we sometimes struggle to have our expertise or importance in the healthcare system recognised,” Dr Montgomery said.
“Look at the Medicare rebate freeze and the proposal to introduce co-payments a few years ago. That would appear to indicate a government not valuing in financial terms and in other senses of the word, the role of GPs.”
A recent article in The New Yorker, penned by renowned US surgeon and medical writer Atal Gawande, contained acknowledgement from the author that prior to his exploration of the issue, he had regarded primary-care medicine as “squishy and uncertain”. He regarded the role of a surgeon as the “real work of savings lives”, with surgery the “definitive intervention at a critical moment in a person’s life, with a clear, calculable frequently transformative outcome”.
If a prominent and respected member of the healthcare community could hold such a view, little wonder that others – governments and politicians among them – are sceptical about the role of GPs in genuinely saving lives and reducing morbidity.
“Unfortunately, GPs are seen as the second cousin in the medical fraternity,” observed Professor Chris Del Mar, professor of public health at Bond University and a GP at Robina on the Gold Coast. “They earn less money, and are looked down upon, not just by the rest of the profession but also by patients.
“It’s a case of ‘just a GP’, which is why it’s so great the college has been moving hard to overcome that,” referring to the RACGP’s campaign and slogan, “I’m not just a GP, I’m Your Specialist in Life’, launched late in 2016.
Now more than ever, RACGP President Dr Bastian Seidel is convinced general practice must be better supported by those decision-makers holding the purse strings. Health should be funded not from the viewpoint of “what we think might make a difference”, but what actually worked, he said.
And that meant continuity of care from the highly-skilled generalist.
“We need a change of mindset,” he told TMR.
For years, mountains of research, most notably from the late US pediatrician and primary care advocate Professor Barbara Starfield, has demonstrated the worth of primary care. But more recent trials have provided the strongest evidence yet that continuity of care in general practice can save not only lives but billions of dollars in expensive, avoidable and, at times, unnecessary hospital admissions. It’s also a better experience for the patient.
One study from the Netherlands, published in the British Journal of General Practice, found adults over 60 who had multiple GPs were 20% more likely to die over the 17-year study period than those who consistently visited the same doctor.
I think a lot of GPs would probably agree that we sometimes struggle to have our expertise or importance in the healthcare system recognised.
Furthermore, UK researchers found patients with the same GP were 12% less likely to be hospitalised with conditions that could have been managed successfully in primary care.
“We’ve had soft data around patient satisfaction and comfort and so forth, and that’s all great but often not good enough to inform health policy,” Dr Seidel said.
“It’s not really about what we like, it should be about what makes a difference to patients and health outcomes. And what works is general practice. We are now getting hard outcome data and that is what we need when writing evidence-based health policy.”
Health policy must include far greater support for primary care from governments who, doctors uniformly agree, are too short-sighted and blinded by the higher-profile, and voter-friendly, world of specialist and hospital care.
According to Dr Seidel, only 5% of Australia’s annual health expenditure of $145 billion goes to general practice, a figure that includes Medicare, practice incentive payments and Primary Health Networks. With 85% of Australians visiting their GP at least once a year – there are 104 million consultations annually – funding was a “measly” $30.40 per person per month, he said.
“That’s how much the federal government spends on GP care,” Dr Seidel remarked witheringly in a recent speech, saying that amount was less than a subscription to Foxtel or The Australian.
Over the same period, hospital funding has climbed 19%.
As Dr Gawande said in The New Yorker, as a surgeon “I have a battalion of people and millions of dollars of equipment at hand when I arrive in my operating room”. GPs on the other hand, “are lucky if they can hire a nurse”.
Furthermore, the respective salaries of surgeons and non-GP specialists appear to mirror that funding disparity.
“We call it almost professional discrimination. The rewards are for fixing up a problem, not for preventing it in the first place and that is the mindset we are dealing with,” Dr Seidel said.
“What we do in general practice is prevent conditions from getting worse. We fix things early. But you don’t hear about this, there is no recognition for it.
“If a patient comes to see me and I diagnose ischaemic heart disease and they are at risk of having a heart attack, I am preventing this by taking action early. But the prevention aspect is just not sexy.
“Politicians are playing to the masses. It’s always a good news story to fund a new hospital or list another expensive drug. If that drug fails five years down the line, well, the money has already been spent when it should have been spent on preventative measures. But unfortunately, that is not politically palatable to a lot of those guys.”
Michael Kidd, a professor of global primary care at Southgate Institute for Health, Society and Equity at Flinders University, said Australia had built a successful healthcare system “on the basis of strong primary care and strong general practice”. Even a cursory glance at markers such as life expectancy, infant mortality and rates of immunisation illustrated that assertion, said Professor Kidd, a past president of RACGP and the World Organisation of Family Doctors.
“We have excellent health outcomes. But there are times when the government takes this for granted,” he said. “What we often see in a time of increasingly scarce health resources, is that resources drift towards that dramatic, heroic emergency intervention and neglects the important role of primary care.”
Among the reasons for the financial skew towards emergency intervention was, Professor Kidd suggested, the weight of “community expectations” where the public, particularly in wealthy countries such as Australia, expected to have access to all the best and latest cures and surgical interventions.
“There is a lot of community pressure, and that is felt by our politicians,” he said.
“Look at the backlash when a political party suggests closing a hospital.
“For those who work in primary care, there are times when they must feel less valued than other parts of the health system.
“That is very unfortunate because they are not less valuable. They are absolutely critical to keeping our population well for as long as possible, and for preventing the need for heroic dramatic emergency treatment.
“We must look very closely at every person who receives that type of intervention, because many will be a result of failures in the health care system that could have prevented the events from occurring in the first place.”
Keeping patients out of hospital is, naturally, one of the fundamental aims of the primary-care system and for GPs individually.
And knowing your patient, establishing a relationship over time and accruing information about their life and circumstances has long been known by GPs as the critical ingredients of succeeding in this aim. It can shape the judgment, treatment and the overall approach to any given problem.
“This is the fundamental part of a GP’s work. It’s that personalised care for a person who through the increments of time you have developed a knowledge of,” Professor Kidd said. “You know their health and well-being, their responses to treatment. You have become their trusted GP. But in primary care there are also heroic dramatic emergency interventions. It’s part of what we do.
“At other times, we’ll be providing incremental treatment to someone with a chronic disease, or providing one-off treatments and cures for those with acute diseases. The primary-care role is complex. It provides comprehensive care and co-ordinated care with other parts of the healthcare system.”
According to another former RACGP president, Dr Liz Marles, a GP in Hornsby on Sydney’s upper north shore, it is this rapport, this long-term continuity of care, that can be undervalued by the wider health community.
But for patients it’s a different story, with the consistency and trust that comes with the familiarity of a single doctor anything but under-estimated.
“They want to have those relationships and want to keep seeing the same GP,” Dr Marles said.
“If I’ve looked after someone for five years I might have spent many hours talking to them about personal issues and circumstances, so when they come in with a problem I’ve got a context for it.
Understanding the whole person makes it easier to determine what’s going on. It becomes a very efficient way to deliver a service.
“I’ll have all the background. I’ll know if they are someone with high anxiety levels or whether they are a stoic who rarely complains. We’ll know what investigations and tests have previously been carried out, what illnesses they have had.
“Understanding the whole person makes it easier to determine what’s going on. It becomes a very efficient way to deliver a service.”
High quality continuity of care at a general practice brought “efficiency of diagnosis”, Dr Marles continued, which was free of duplicate tests and unnecessary medications “because we don’t bark up the wrong tree”.
Non-GP specialists have, of course, unparalleled expertise in their respective fields, but by the very nature of their narrow focus, rarely approach a patient from a holistic viewpoint – a strength of the generalist.
If a specialist finds nothing of concern in their own area of expertise, it is entirely possible the patient could be shunted to another department and, according to Dr Marles, at risk of “having a whole lot of inappropriate” tests.
“They are not really trained in that broad initial work,” she said. “Most diagnoses take place in general practice. If someone comes in with a headache or abdominal pain, the GP will be thinking broadly and be able to ask the appropriate questions, do the appropriate tests and narrow it down.”
One of Dr Brett Montgomery’s students told him she was almost in awe of the extraordinary depth of knowledge required by a GP, telling him it was just too hard and she needed to narrow herself to a certain field, in her own case anaesthetics.
“It was one of the nicer things to hear,” he said.
Professor Del Mar echoed the thoughts of Dr Marles, arguing that continuity ensured “the right things are being dealt with” while at the same time preventing cases of polypharmacy by weaning patients off drugs that might have outlived their usefulness.
“We deliver care that keeps people away from expensive high tech medicine that very often they don’t need,” he said.
He tells the story of a patient who had seen him the previous day complaining of chest pains, his anxiety heightened by the recent death of a relative from a heart attack.
In his case, a visit to an emergency department, unfamiliar with his history, may have led to an ECG, X-rays and even a precautionary hospital admission – all at significant cost and additional stress.
Professor Del Mar examined his patient, found little of concern, and offered gentle reassurance that nothing serious was amiss. Within half an hour, his patient had departed, relieved and comforted and without a needless visit to a coronary-care unit.
“What GPs are good at is communication. One of the things we are taught is the patient-centred communication system. In other words, make sure you understand what makes your patient tick, what are they frightened of, what concerns them. If you know these things you can address them.”
Yet all this was at risk of being undermined by funding issues, exacerbated by the long-standing Medicare rebate freeze which, said Dr Marles, had piled pressure on already-stretched GPs.
With some practices financially struggling, the pressure to see more patients has intensified, leading to shorter consultations and, ultimately, less time to effectively manage the patient. This in turn can lead to an increased number of referrals.
In New South Wales alone, 20,000 extra patients descended on emergency departments in the October to December quarter compared with the same period in 2015, although how much of this increase can be attributed to the freeze cannot be ascertained.
“We have had a fantastic system in this country. Primary care has been really well developed … the skill set of GPs is very high, but I think the issue has been the system has not supported them to work to that skill set. We are getting more and more care shunted, at cost, to the specialist end of things rather than allowing GPs to use their skills to keep the costs down.”
As you might expect, Dr Seidel said GPs were the most trusted of all health professionals. Patients, he said, “want health, not necessarily treatment”, with a strong doctor-patient relationship likely to result in fewer medications, less diagnostic testing, fewer pathology tests, and ultimately, fewer hospital admissions.
In addition, if all patients saw their GP within a week of hospital discharge, readmissions would be reduced by 23%. This could be easily achieved if there was the political will, said Dr Seidel.
Flinders University’s Professor Kidd said while a strong healthcare system could be taken for granted, governments around the world, including Australia, had “rediscovered” the importance of high-quality primary care, which was pivotal to meeting the challenges posed by the rise of non-communicable diseases such as diabetes and heart disease.
Primary care held the solutions through early detection and appropriate management, he said, to prevent these conditions reaching the point where they become life-threatening.
And so it circles back to Dr Montgomery and his students in WA, attempting to travel back in time to the day his patient was saved from his future.
We need to change the mindset. We can’t afford the shiny treatment stuff anymore. It is costing us so much.
Consultants, surgeons and emergency intervention may grab the attention, plaudits and the lion’s share of resources, but primary care is where the real difference can be made, as more hard data seems to confirm.
“We need to change the mindset,” Dr Seidel said. “We can’t afford the shiny treatment stuff anymore. It is costing us so much. We should be focusing on what works, and what works is general practice and we have the track record to back it up.”
Whether performing in-practice procedures, identifying warning signs of potential future ill-health through opportunistic or continuous care, offering reassurance and guidance, or managing conditions over a long period of time, GPs are as much at the cutting edge as emergency intervention, probably more so.
As Dr Marles concluded: “I get a lot of satisfaction from the longer-term nature of the doctor-patient relationship and I get to see some fantastic outcomes in terms of people getting better and better. It’s a one-on-one relationship, and my patients are often incredibly grateful.”
The primary care sector must hope more people – in particular those in influential positions – soon become similarly appreciative.


