A Sydney GP with an interest in long-acting reversible contraceptives says accessibility during the postpartum period is still too low.
The RACGP may have come out against a new item number for endorsed midwives who insert long-acting reversible contraceptives (LARCs), but proponents of the idea argue that not all scope expansion is necessarily bad.
Earlier this month, the RACGP published its submission to the MBS review advisory committee LARC working group, which is currently considering whether to expand MBS funding to a subset of midwives who insert or remove LARCs.
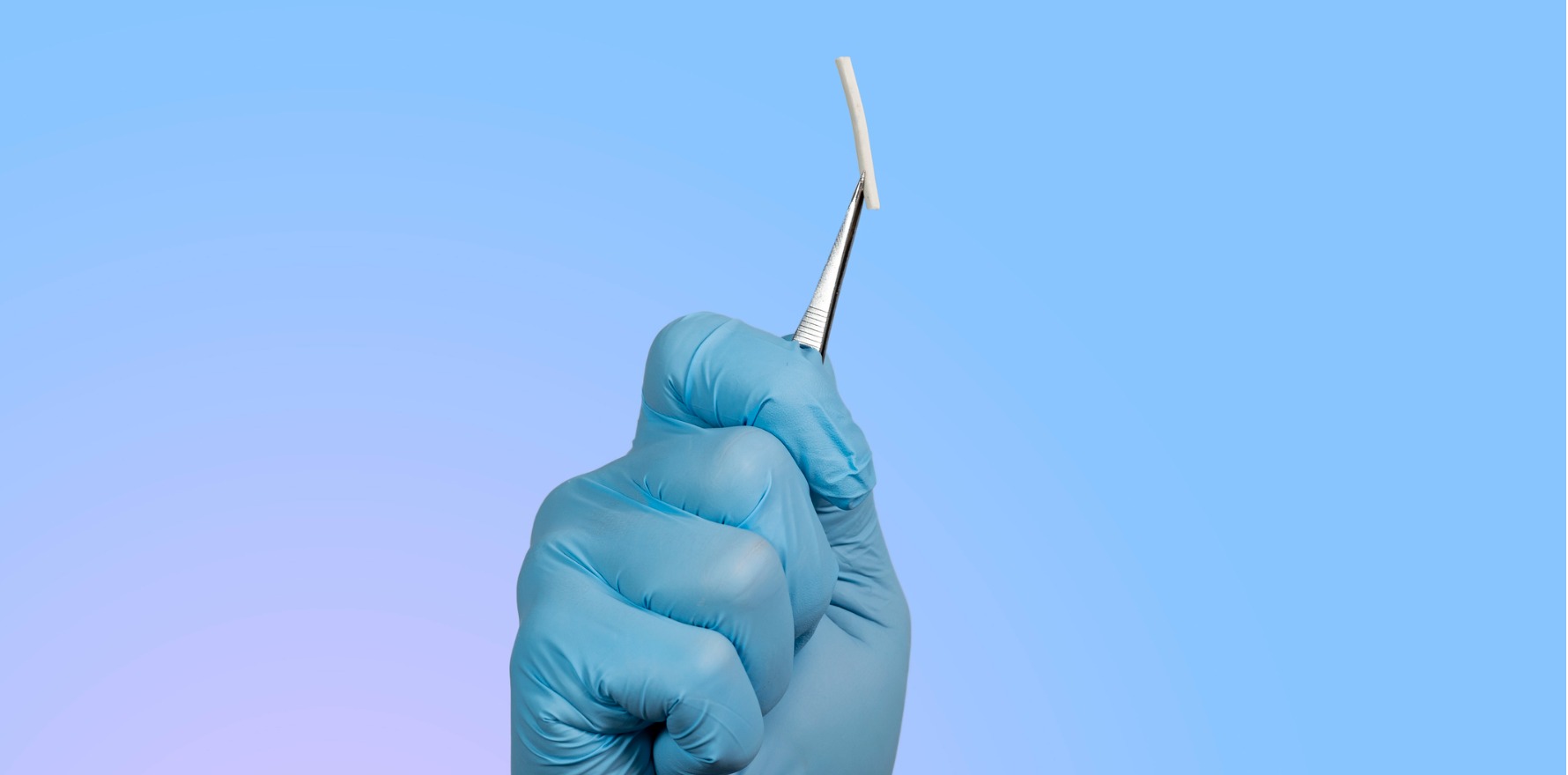
In its submission, the college warned that “although LARC insertion may appear to be a simple procedure to some patients and non-medical practitioners … it involves inherent clinical risks and may present substantial procedural complexity in particular circumstances or patient population risk”.
Sydney GP Dr Sneha Wadhwani, who is the clinical director of Evoca Women’s Health (a subset of GP corporate ForHealth) told The Medical Republic that midwives were well placed to treat women in the immediate postpartum period, provided they were given the same LARC training as a GP.
“They are already trained in reproductive and contraceptive care in Australia anyway, and they are talking to women around this topic,” she said.
“I think this is just an extension of that scope. And if you look internationally, lots of countries in the Western world do adopt the LARCs far better than we do here in Australia.”
Related
Around one in three women in Sweden, for instance, use a LARC. In Australia, this figure is closer to one in 10 women.
“We know that the barriers to [uptake] are cost and also the availability of fitters,” Dr Wadhwani said.
“And this is why Evoca has its own in-house training … for us, enabling midwives to do this just improves access for women, in view of Australia having the lowest uptake in the Western world.
“And I think we’ve got to be aware that these new MBS items and incentives around LARCs are likely to drive demand.”
Dr Wadhwani said that while there were some women who did not want to talk about contraception in the immediate postnatal period, there were often others who were certain that they did not want more children.
“For them, actually capturing this opportunity to place something like the contraceptive implant or even just discuss long-acting, reversible contraception with a view to fitting at a later date is actually a really positive thing,” she said.
“If you think also about our more vulnerable women who’ve had children – there might be a domestic violence situation, there might be drugs and alcohol, they might be very young mums – coming into a GP practice has all sorts of connotations and concerns for some of them.
“And if they’ve got a relationship with a health practitioner who’s looked after them through their pregnancy, then that’s a really positive thing. I think there’s a real important role here for this.”