Nuances in rollout, laws and the demographic and geographical landscape mean that it’s shaping up differently across the country.
Australia’s inaugural Voluntary Assisted Dying National Conference took place in Sydney last week, bringing together the who’s who of VAD services to discuss, among other things, the VAD landscape as it stands across Australia’s jurisdictions.
Voluntary assisted dying is now a legal option for competent, terminally ill adults in Queensland, South Australia, Victoria, Western Australia and Tasmania, with New South Wales to join as the sixth state towards the end of the year.
The basics
All states and territories that have current legalised VAD require eligible people to be 18 or over, have decision-making capacity, be acting voluntarily and have a terminal medical condition likely to cause death within six or 12 months. (Neurodegenerative conditions are the exception to the six-month rule, except in Queensland, which allows all patients expected to die within 12 months to apply.) In Victoria, SA and Tasmania the illness must be incurable, and in Tasmania it must be irreversible.
States generally require a person to request VAD at least three times, and to be assessed for eligibility by at least two authorised practitioners.
Only Australian citizens or permanent residents are eligible – exceptions are possible in Tasmania, Queensland and NSW – and most states require at least 12-month state residence.
VAD can either be self-administered or practitioner-administered. In Victoria, SA and Tasmania VAD must be self-administered, unless the person is incapable. In Queensland, WA and NSW it is the patient’s decision which process to use.
While the process may differ slightly, the outline remains consistent for most states.
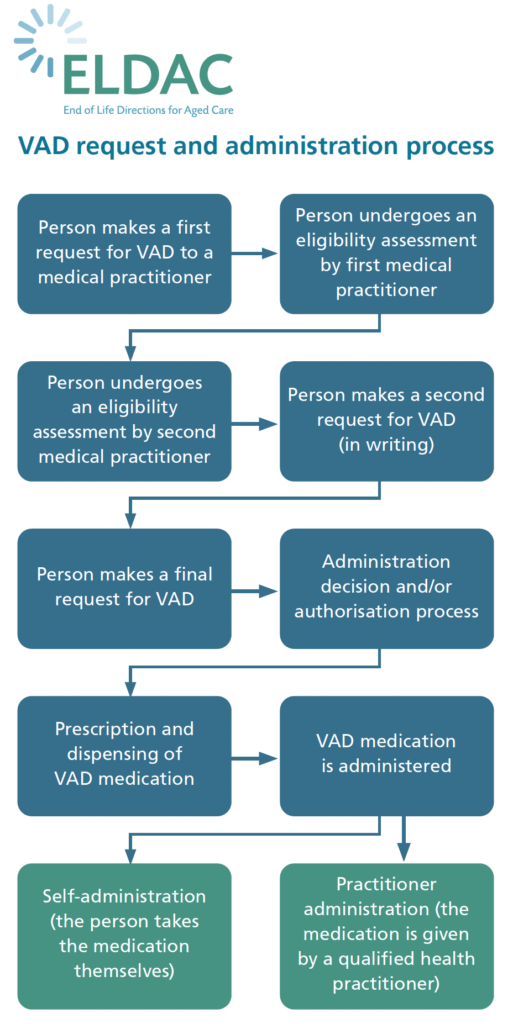
Process in Victoria, WA, SA, Queensland and NSW. Tasmania has additional requirements. Source: eldac.com.au
But the legal rights and obligations of health professionals differ state by state.
While in Victoria and SA medical practitioners cannot initiate a VAD conversation, WA, Tasmania, Queensland and NSW allow practitioners to initiate the conversation but they must also discuss other treatment options.
In Tasmania and NSW, other registered health practitioners can also initiate the conversation, but they must note that the patient should talk to a medical practitioner for more details.
All health professionals may conscientiously object to participating in VAD services, but in WA, Queensland and Tasmania they must provide contact details of where services can be sought.
Victoria
Victoria was the first state to successfully pass and enact VAD legislation in Australia that still stands. The law came into effect on 19 June 2019.
In the initial three years of the service, 604 people have been assisted to die by the now 326 trained registered medical practitioners offering the service.
Of the active providers, 70% are GPs. The rest of the registered practitioners include specialists in oncology (16%), neurology, general medicine, respiratory and sleep medicine, haematology, palliative care and other.
Victoria was also home to Australia’s first organ donation after VAD.
Marlene, who opted for VAD after a diagnosis of motor neuron disease in late 2022, was able to provide five people with lifesaving transplants, according to Larna Woodyatt, a donation specialist nurse for DonateLife, who spoke at the conference.
DonateLife Victoria has now developed organ donation guidelines, which should be “transferable” to other states and help them to start to facilitate organ donation, said Ms Woodyatt.
Queensland
VAD became available to Queenslanders on 1 January this year.
Speaking at the conference, Professor Liz Reymond, director of Queensland Voluntary Assisted Dying Support Service (QVAD), spoke on the uptake for the service among health professionals.
While a “pretty good” 168 practitioners are offering services as of 19 September, the prescribers are “disproportionally scattered across Queensland” with a few carrying most of the load.
“All credit to the Queensland Health van unit who put in an enormous amount of effort to get to that point with the training and the recruitment,” Professor Reymond added.
Out of the 618 scripts written over the initial nine months, which she said “far surpassed” the expected demand, 32 prescribers had written five or more scripts, while the majority of prescribers had not written any.
According to QVAD’s data, 19% of the authorised prescribers are providing 88% of the VAD services.
“That represents a very significant potential for burnout and that threatens our sustainability for setting up a service,” said Professor Reymond.
There is also significant variation in prescription of oral versus IV-assisted.
“I find it hard to believe that that’s based on case distribution or patient choice – I can’t help but think that there’s a little bit of practitioner preference sneaking in there,” said Professor Reymond.
At present, according to the data, only four private entities are scripting, meaning there was a heavy reliance on public service “until we get more MBS numbers”.
Part of QVAD’s service helps link patients who are unable to find a suitable practitioner. The top three areas that require assistance were rural and remote areas, demonstrating the importance of changing the criminal code to allow telehealth VAD services, she said.
South Australia
The Voluntary Assisted Dying Act, which was passed in 2021, commenced in SA on 31 January 2023.
Kyam Maher, the Attorney General and Minister for Aboriginal Affairs in South Australia, said that within the first three months of the service, 28 South Australians had been accepted for VAD, 11 had passed away from their use of VAD and one had passed away from natural causes before using VAD.
Mr Maher said carers and relatives had told him how much difference it had made to their lives: “the fact that their loved ones had some control of the end of their life, and the dignity that that provided for all of them.”
Western Australia
VAD legislation came into effect July 2021 in Western Australia.
In its first annual VAD report, issued in November of last year, the demand for VAD had been greater than expected the WA VAD Review Board said.
“Though a complex process, the ability of Western Australians to make the lawful choice of voluntary assisted dying, and to traverse the steps required to fulfill that choice, has worked well under the Voluntary Assisted Dying Act 2019,” said board chair Dr Scott Blackwell.
In the 12-month period, 190 people administered the VAD medication, totalling 1.1% of all deaths in WA in that time.
Similarly to other jurisdictions, almost 80% of access was concentrated to metropolitan areas.
Out of the 70 doctors and nurse practitioners who had completed training, 50 were actively assessing patients.
“The Voluntary Assisted Dying Board is concerned about the personal and professional pressures this places on participating practitioners. More participating practitioners are required to meet this greater than expected demand,” the annual report noted.
Tasmania
Tasmania’s VAD scheme began in October 2022, making it the third jurisdiction to offer VAD services.
In its first four months of operation, 24 initial VAD requests were made, 11 were authorised and five people died through the VAD process.
Tasmania’s VAD commission hailed its “positive” number of authorised practitioners, considering its small size and limited practitioners, in a statement earlier this year.
“Of the 23 medical practitioners who completed the training, 16 indicated they were willing to be Primary Medical Practitioners and/or Consulting Medical Practitioners. Of the 21 registered nurses, 15 indicated that they were willing to be Administering Health Practitioners,” the statement read.
New South Wales
New South Wales will be the next jurisdiction to allow VAD.
Services will be accessible in NSW from 28 November.
However, application to be an authorised prescriber can be made through the NSW Voluntary Assisted Dying Portal.
Speaking at the inaugural national VAD conference, NSW Heath’s VAD clinical lead Dr Wade Stedman said that they expect 1200 people to access and use VAD services in the first 12 months of the program.
Dr Stedman is hoping that the state’s face-to-face training will help encourage practitioners to be involved in a somewhat daunting service.
Northern Territory
Despite being the first jurisdiction in the world to legalise euthanasia in 1995, after the bill was quashed only two years later the NT will now be the last to reintroduce voluntary assisted dying.
Last year, the NT’s right to legalise VAD was restored by the federal government after the Restoring Territory Rights Act 2022 was passed in December.
The Territory’s government has since established a panel of advisors to consult on the role out.
The consultation is expected be completed by July next year, she added.
Australian Capital Territory
Alongside the NT, the ACT has not yet passed VAD legislation.
However, ACT Minster for Human Rights Tara Cheyne confirmed at last week’s conference that a bill will be introduced in the state before the end of this year.
The state plans to take a “considered” approach, learning from other states said Ms Cheyne.
Major variations will include doing away with the mandatory timeframe until death, that for most states stands at 6-12 months, as these estimations can result in “unfair outcomes” and this change is unlikely to result in more people become eligible for VAD, they may simply be eligible sooner.
Additionally, due to “strong” support, nurse practitioners will be eligible to be coordinating or consulting practitioners if the other practitioner involved is a medical practitioner.





