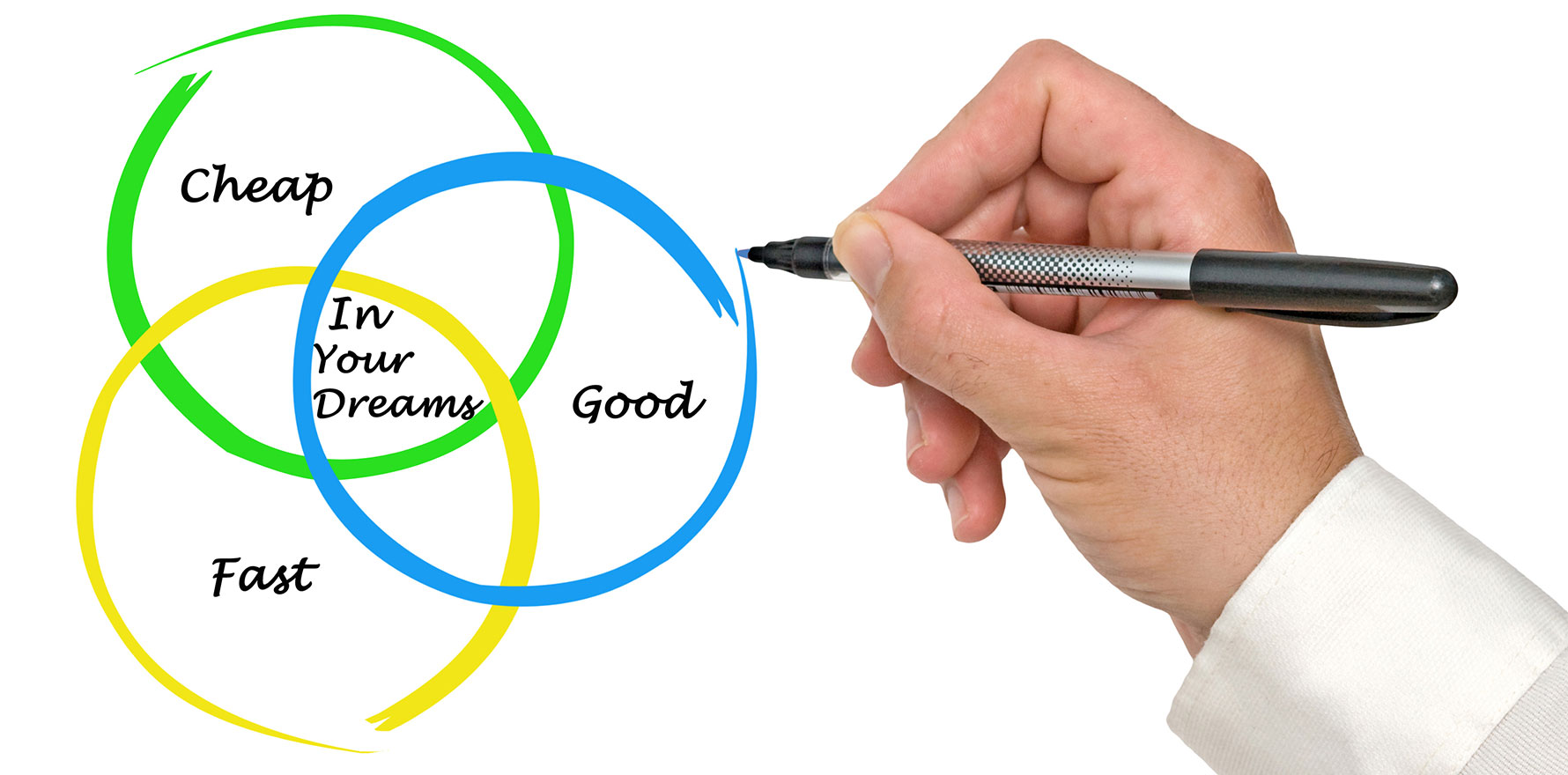
The ‘you get what you pay for’ attitude exists on both sides of the consulting room.
I had a once-in-a-lifetime opportunity last month to attend a business conference by esteemed Swiss dermatolgist Dr Felix Bertram, who has many claims to fame, including multiple clinics in his home country.
While the bulk of the conference may be unrelated to general practice in Australia, one part of it struck me the most – Felix’s “why”.
As he says it, medical care in Switzerland is covered by public insurance and free at the point of care. He was motivated to revamp his clinic, and then clinics, by the desire to provide an elevated service to his patients.
In his experience, the fact that waits were days to weeks to access a doctor, and service was often basic if not poor, was motivation for him to provide a better experience for his patients at every touchpoint.
What he set out to achieve is something to behold and left me aspiring to do even better than I currently am back home.
But that is not the point I’m hoping to spell out here.
For decades, general practice and indeed, many GPs, have possibly ridden the coattails of universal bulk billing (UBB) to provide suboptimal care to our patients, comfortable in the knowledge that as long as care is “free” at the point of care, patients will likely continue to attend our practices.
In recent years, as most of us have moved away from bulk billing, whether out of necessity or other motivations, there have been many heated arguments in internet forums about the ethics behind this, as well as whether we are providing adequate care to “deserve” charging a gap fee.
One has only to look at any media article over the last few years to see how bitter the debate is over this issue among the public – used to “free” care, no matter how basic – now that they have to pay for it, and how scathingly they speak of the care provided by ostensibly ALL GPs.
For those of us who relied on universal bulk billing to keep our practices running, this is possibly the first time we have to put some thought into what we might have to do to keep patients coming back to see us if there is even a minuscule gap fee involved.
The fact that care has been “free” has allowed a “you get what you pay for” attitude.
I left UBB in 2013 in large part because as a GP trainee, every one of my training practices was UBB and I was frequently encouraged to do things that were against guidelines to “keep customers happy or else they’ll just go to the practice next door and we’ll lose them”.
I lost track of the number of times I reminded my supervisor “they’re not customers, they’re patients”.
Related
So for my own sanity as much as anything else, I decided I wanted to work differently. I wanted to do good work, take my time and work with the patient. And I wanted to charge for my time and expertise if they were able to pay and let them decide if the service was worth paying for.
Every person I spoke to, when I decided to test this out as a final-term registrar awaiting fellowship, told me it was a bad idea: I’d suffer for it, cost the practice custom and come up short myself (because I was not an employee). I did it anyway, and it worked.
In theory, I believe firmly in universal access to healthcare.
In practice, based largely on having now spent over a decade watching how it plays out in reality, I tend to agree with the psychologists – what we get for free, we don’t value; both as providers and patients alike. Even a small exchange of money confers greater value and accountability.
But with Medicare being what it is now, that decision has largely been removed from most of us wishing to stay afloat with our small businesses.
Learning about Dr Bertram’s practices, I was struck afresh by the similarities between their system and ours in times gone by when the patient rebate was “plentiful”; and the inevitable malaise that seemed to accompany “free” care in the last decade when patient rebates were frozen.
While it is undoubtedly bad for patients in real need who are hard pressed to pay a gap fee to access a good GP, it can be equally true that for most of us, having an attentive GP who truly is invested in helping us make a difference in what ails us, even if it means a gap fee, is likely better and paying these fees may enable them to have a few spots in their week to see those who are genuinely disadvantaged if they wish to.
The debate will rage on, between those who believe that access to a good GP is a universal right, full stop, and those who say this is only true when the providers are properly remunerated and not paying for patients out of their own pockets.
Dr Imaan Joshi is a Sydney GP; she tweets @imaanjoshi.