We all want to do something, but whether through incentives or education, GPs are not the lever to press to bring about change.
Recently, there has been a proposal to add yet another item number to an already burgeoning tome of billing options in the MBS.
The idea is that adding more money to an activity will motivate GPs to spend more time doing it. The reasoning goes that financial incentives will drive activity, and activity will drive change. This works in marketing things we can sell, but I have my doubts that it will work with item numbers. The reasons are complex, but in my view, there are profound disincentives to using incentives at all. Here are a few.
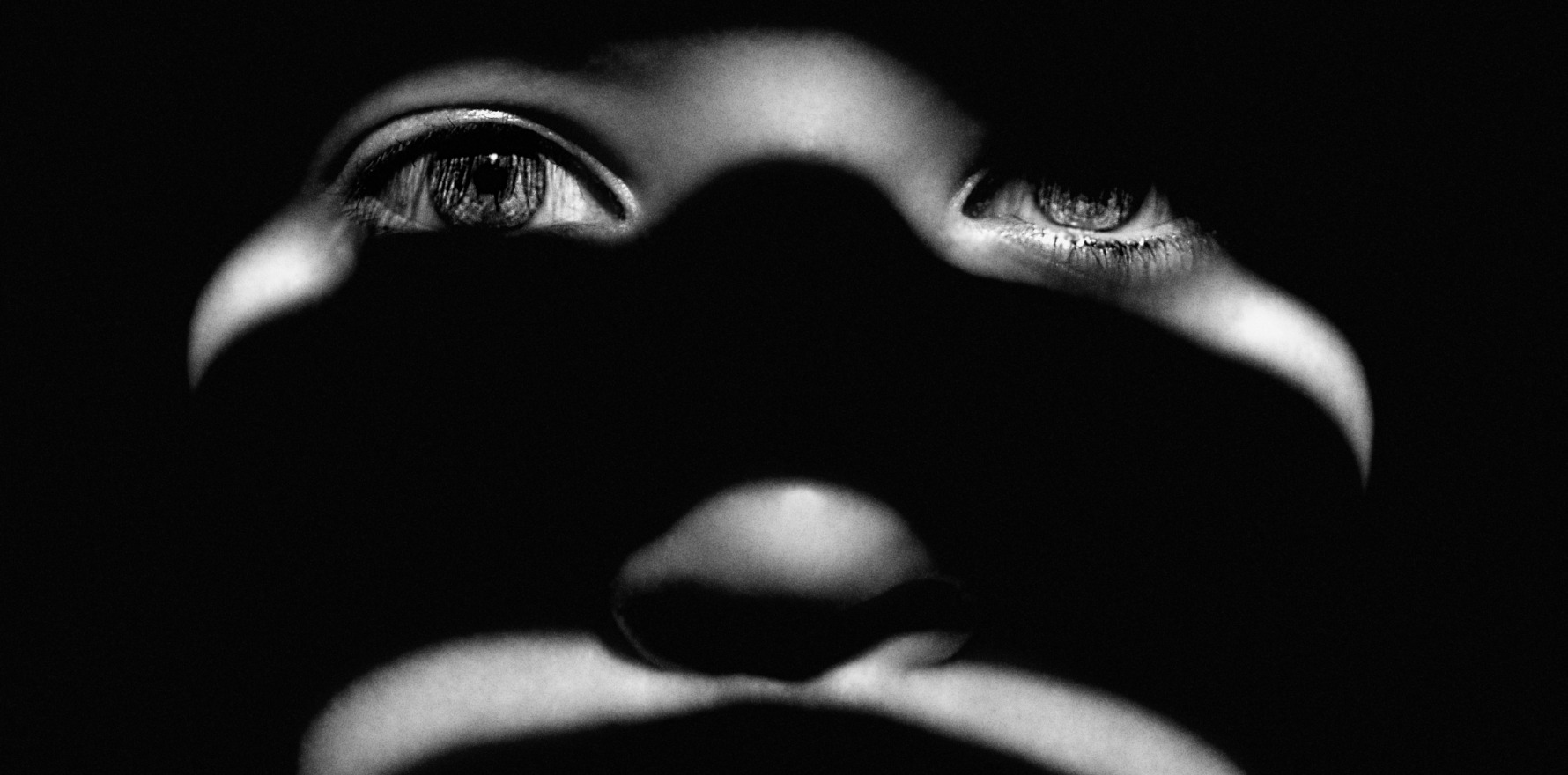
Fear
In general practice, there has been sustained activity by the behavioural economists to drive change using fear. The nudge letters, with their hidden threats of the PSR, have driven GPs to avoid trying to maximise rebates. The rebate goes to the patient, of course, not the doctor. This means that once we abandon bulk-billing, maximising rebates becomes less of a motivation.
It is the patient who gets the rebate. If GPs balance the fear of the nudge, or the PSR, and/or the fear of AHPRA against obtaining a few extra dollars for their patients, many will simply not try to use anything that can be misinterpreted. We have not forgotten the strident allegations of fraud that led to escalating abuse and violence from patients in our practices who accused us of “rorts”, and we need to protect our vulnerable staff.
Safety
Patients experiencing domestic violence are beyond vulnerable. Many pay me in cash because their partners know all of their passwords and monitor their Medicare accounts. It takes one GP to bill this number, with or without the patient’s consent, and there will be an excuse for a beating, or worse, another death. What’s more, in some communities, the perpetrator knows where the doctor lives and works, and knows where their children go to school. Policy makers need to consider our own mantra: first do no harm.
Motivation
There are two problems with motivation. The first is the idea that motivating GPs to do more work in this space using a carrot (financial incentives) or a stick (compulsory education) will change outcomes for patients. Not necessarily so. Domestic and family violence is covered well in the curriculum. We teach it, examine it, and supervise registrars managing it.
The problem is one of capacity. In policy, one of the first questions to ask in health is this: “can the best, most motivated, most educated GP in this field make a difference under this policy”? If the answer is no, then we need to rethink.
In this case, I suspect the rate-limiting step is not the GP. If there is no refuge, no safe haven for the children, no safety for the mother (and it usually a mother) and no justice in the Family Court, then motivating, incentivising and educating me makes little difference.
The next problem with motivation is why we are suggesting this in the first place. With a wicked problem like family violence, there is a sense of enormous helplessness. There is a famous saying that for every complex problem, there is a simple solution that is neat, plausible and wrong.
In teaching, it is always the primary school curriculum. Deaths on the roads? Put road safety in the primary school curriculum. Drownings? Add swimming lessons. Sexual abuse? More teaching on consent. In health, it is educating, motivating, shaming and incentivising GPs to “do more”. It doesn’t work. Our curriculum is enormous. Our CPD burden is enormous. Adding more to it will not change the fundamental problem that this is the wrong lever to enact change.
Compassion fatigue
We have been propping up the system with compassionate donations of time and labour for decades. It is no longer sustainable. Like any situation where there is sustained abuse, eventually the survivor realises that trying to meet ridiculous and conflicting demands isn’t sustainable and makes no difference in the end.
At present, we remain in this intolerable mess for the sake of the patients. Like many women, women doctors continue caring for more vulnerable members of the tribe by filling gaps with empathic care. However, we have hit a watershed. Women doctors, with their excess load of chronic disease and mental health care, and their burden of emotional and financial exploitation, are leaving. Many are suffering. Some are dying. A light sprinkling of extra funding will not change the broken system and does not begin to recognise the depth of abuse that is occurring within the Medicare system.
Fragmentation of care and billing
There is an old idea in medicine that refuses to die. The idea is that medicine is one great big lump of knowledge and understanding. If we could understand every single particle of this lump, we would understand the whole.
This is patently not true. I have never seen a biochemist attempt to solve structural inequity in society, or population interventions for infectious diseases, but I suspect they would not provide the best response.
Similarly, we will not provide the best healthcare solutions by replicating the coding we see in hospitals. It works with procedures. I can pay for this patient because their service includes a colonoscopy, a form of abdominal surgery and a loading for each of their chronic diseases that complicate their care.
In general practice, it is nonsense. Send me a patient with five chronic diseases, poverty, a history of trauma, chronic pain and neurodiversity, and, instead of today’s Wordle, listen to me run the consultation and try to quantify which minutes I spend on which issue. It is impossible, and what’s more, it is utterly meaningless. Then imagine me trying to do it while managing that patient, with the threat of the PSR and the nudge, and you will see what I mean.
Prestige
The most important part of this debate is the one about prestige. Who gets to decide what a patient is worth, or what their issue is worth, in the MBS schedule? Why is a patient who is assaulted by her husband “worth” more than a woman who is assaulted by a neighbour? Why does a person who needs a skin excision receive a higher rebate for their consultation than a person with depression? Why are activities that women GPs do (complex mental health and chronic disease) worth less to the community than procedures? And before we say that procedures carry the cost of equipment, there is no loading to do cervical screening tests.
To make is even more concrete, why is it, when I do six-minute medicine I attract $6 per minute for the practice, but when I see an adolescent sleeping in their car for their deep mental health needs, it’s around $1.25? Why are GPs doing this complex work worth so much less for doing so much more?
The answer is in disease prestige. All suffering is valid, but some suffering is more valued than other suffering. When I had young children, I had reason to spend time in the Royal Childrens’ hospital in Melbourne. At the time, it was a multistorey building. On the third floor was the cancer ward. There was a hand-carved rocking horse, bespoke equipment, commissioned art and a number of publicly funded therapists or various sorts. As you went up in the lift, the diseases were less and less prestigious. On the top floor, children suffered just as much with their solid organ transplants, cerebral palsy and renal failure. But the wards were bleak, and the only decorations were dusty old paintings and a fish tank with a solitary fish, swimming endlessly in circles.
Someone has to be brave enough to make the MBS equitable. The executive should not get six times the rebate for his flu vaccine that my patient gets for his suicidality. Because, inevitably, this means the executive finds it easier to access bulk-billed services. Similarly, why would we set up a system where the source of violence (in this case, within the home) changes the worthiness of care? It makes no sense.
The reason, of course, is we want to DO something. We want to demonstrate that we are taking this issue “seriously”. We want to announce something that indicates we are “helping”. This is not fair, equitable or just, and it means that conditions with power (lobby groups, famous advocates, political expediency) will get more support than conditions that attract little respect, awareness or support.
What’s more, it compounds. Cancer is important. It attracts a lot of philanthropy, research funding and healthcare dollars. It has reason to. It is common, people understand it, and the visuals are easy to market. But the incontinence scheme also makes an enormous difference. There will never be a fun run for incontinence.
Governments need to be brave enough to argue for the just funding of all people who need support, not just the ones the public understand. The domestic violence item number is yet another example of where one form of suffering, horrible though it is, is supported more than other equally horrible forms of suffering. This is not good enough. We can do better and we should.
Associate Professor Louise Stone is a working GP, and lectures in the social foundations of medicine in the ANU Medical School. Find her on Twitter @GPswampwarrior.