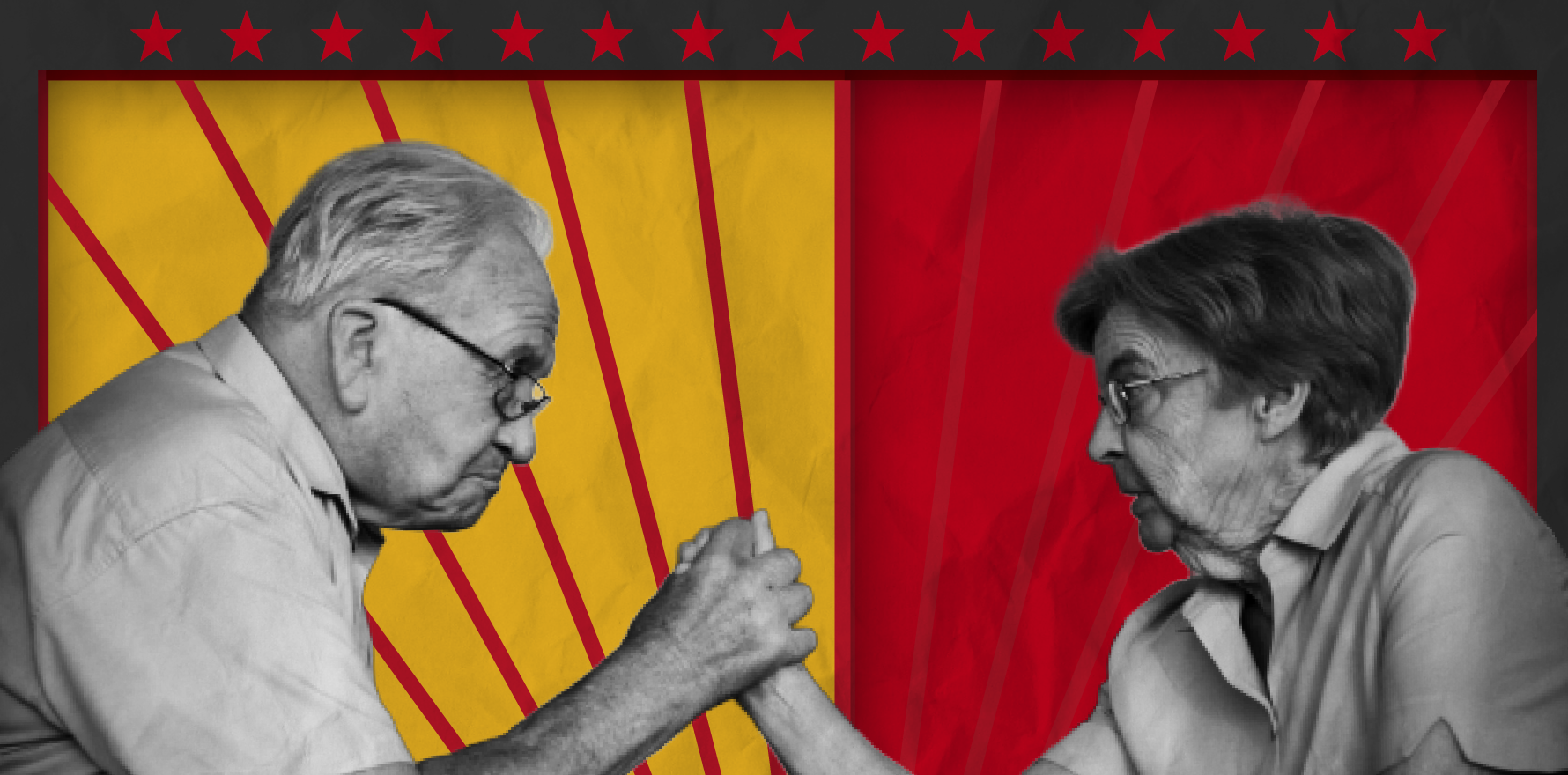
To prescribe or not to prescribe anticoagulants in atrial fibrillation can be a fraught decision.
One of the more challenging clinical decisions we face as GPs is whether to prescribe oral anticoagulants for patients with atrial fibrillation (AF).
And it’s no small issue – AF is the most common recurrent cardiac arrhythmia, affecting over 500,000 Australians, and it plays a role in nearly one in 10 deaths.1 Despite this, many patients with AF remain undertreated, with only about half of eligible individuals receiving anticoagulation therapy.2
The hesitation to prescribe anticoagulants is largely due to the uncomfortable tension between preventing a stroke and triggering a serious bleed. This decision often feels like a double-edged sword, particularly in older, frail patients or those at risk of falls.
However, the statistics are hard to ignore. AF increases stroke risk five-fold, and those who suffer a stroke in the context of AF often have larger infarcts, more disability, and worse outcomes.3,4 Yet, anticoagulation with either warfarin or direct oral anticoagulants (DOACs) reduces stroke risk by 64% and all-cause mortality by 26%.5
So if the benefits are clear – what’s holding us back?
Research has highlighted significant variation in anticoagulant prescribing for AF. Rates range from 39% to 66% across general practices,2 and while rates of prescribing have improved over time, many patients remain untreated.2
The reasons for this are complex and familiar – and this list is by no means exhaustive:
- Fear of bleeding
Clinicians often overemphasise the risk of bleeding, and focus heavily on bleeding risk scores to justify withholding anticoagulants. Current guidelines are explicit: the benefits of stroke prevention nearly always outweigh the risks of bleeding.6 Rather than using bleeding risk as a reason not to treat, we should use it to guide the mitigation of modifiable risks. - Age-related caution
Understandably, many GPs are cautious about prescribing anticoagulants in elderly, frail, or cognitively impaired patients. While falls risk is important, the evidence shows that stroke risk increases with age at a greater rate than bleeding risk.7 - Access challenges
Accessing cardiologists in the public system, and long wait times can also lead to delays in appropriate anticoagulation. The reliance on specialists for a second opinion is commonplace as many GPs have concerns about initiating treatment. In rural and remote areas, the access issue is even more pronounced. - Anticoagulant selection and dose modification
Uncertainty about the pros and cons of different anticoagulant medications and dosages for individual patients can lead to hesitation, especially in the context of renal impairment, extremes of body weight and frailty.
Patient concerns (including financial) and misconceptions can compound clinical hesitation further, contributing to underuse of anticoagulants even when they are clearly indicated.
Many patients view anticoagulants as dangerous “blood thinners,” while underestimating the devastating impact and risk of stroke. As a result, adherence and persistence are poor – Australian PBS data shows only 57% of patients remain on treatment at 2.5 years.8
DOACs are convenient – no INR checks and fewer drug interactions than warfarin – making them easy to prescribe. However, it’s important that this does not result in a ‘set and forget’ approach. Without regular follow-up, patients may not appreciate the need for continued adherence and changing clinical factors, such as renal function or body weight, often go unchecked, leading to inappropriate dosing and reduced treatment effectiveness in the longer term.
It’s small wonder then that the decision to prescribe anticoagulants remains fraught and that under prescribing is commonplace.
Getting to grips with the problem
Recognising the scale of this issue, the Australian Government has funded the Quality Use of Medicines Alliance to improve the management of AF and use of oral anticoagulants. The Alliance – a collaboration of organisations including Medcast (of which I am a founding director), RACGP, Pharmaceutical Society of Australia, research organisations and consumer groups – has developed a national education program for GPs, nurses, pharmacists, and patients.
The program provides:
- tools and guidance for assessing stroke and bleeding risk;
- guidance on initiating and reviewing anticoagulation including anticoagulant selection and dosing;
- strategies for managing complex cases, perioperative care and transitions into aged care;
- shared decision-making aids and patient-friendly resources;
- educational outreach, webinars, and case-based learning for primary care teams.
The program also addresses long-standing knowledge gaps, such as the limited role of aspirin in stroke prevention. Importantly, it supports patient-centred discussions and informed choices that move beyond the fear of bleeding.
Stoke prevention must prevail
Ultimately our goal is simple but critical: fewer strokes. Preventable strokes due to untreated AF continue to occur, and every missed opportunity to anticoagulate is potentially a life changed forever.
This new program doesn’t promise to make the decision easy or to end the arm wrestle. But it aims to make it clearer, more evidence-based, and more collaborative. The challenge of balancing stroke prevention with bleeding risk won’t go away, but with the right tools and conversations, we can do better for our patients.
This free national educational program is now available through Medcast’s QHUB platform.
For more information visit QHUB
Stephen Barnett
Clinical A/Prof Stephen Barnett is the Managing Director of Medcast, a GP in the Southern Highlands of NSW and an experienced GP supervisor and Medical Educator.
He is a Clinical Associate Professor with the University of Wollongong Graduate School of Medicine and holds a PhD in e-learning and GP Training.
References:
1. Australian Institute of Health and Welfare. Heart, stroke and vascular disease: Australian facts. 2024 Oct 12; Available from: https://www.aihw.gov.au/getmedia/61010c29-cd66-46c7-9d7d-de590c0c7788/heart-stroke-and-vascular-disease-australian-facts.pdf?v=20250108111512&inline=true
2. Bezabhe WM, Bereznicki LR, Radford J, Wimmer BC, Curtain C, Salahudeen MS, et al. Ten-Year Trends in the Use of Oral Anticoagulants in Australian General Practice Patients With Atrial Fibrillation. Front Pharmacol [Internet]. 2021 Mar 23 [cited 2025 Jan 10];12:586370. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8044929/
3. Kim J, Nivelle E, Dalli LL, Zomer E, Birhanu M, Purvis T, et al. Economic Impact of Stroke Report 2024 [Internet]. Monash University; 2024 Sep [cited 2024 Dec 20]. Available from: https://bridges.monash.edu/articles/report/Economic_Impact_of_Stroke_Report_2024/27049219/1
4. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991 Aug;22(8):983–8.
5. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007 Jun 19;146(12):857–67.
6. Topic | Therapeutic Guidelines | Atrial fibrillation and atrial flutter [Internet]. [cited 2024 Nov 18]. Available from: https://tgldcdp.tg.org.au/viewTopic?etgAccess=true&guidelinePage=Cardiovascular&topicfile=atrial-flutter
7. Fox KAA, Lucas JE, Pieper KS, Bassand JP, Camm AJ, Fitzmaurice DA, et al. Improved risk stratification of patients with atrial fibrillation: an integrated GARFIELD-AF tool for the prediction of mortality, stroke and bleed in patients with and without anticoagulation. BMJ Open [Internet]. 2017 Dec [cited 2024 Nov 5];7(12):e017157. Available from: https://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2017-017157
8. Simons LA, Ortiz M, Freedman B, Waterhouse BJ, Colquhoun D. Medium- to long-term persistence with non-vitamin-K oral anticoagulants in patients with atrial fibrillation: Australian experience. Curr Med Res Opin [Internet]. 2017 Jul 3 [cited 2024 Nov 19];33(7):1337–41. Available from: https://www.tandfonline.com/doi/full/10.1080/03007995.2017.1321535