The MBS review is targeting more than just “low-value” GP items
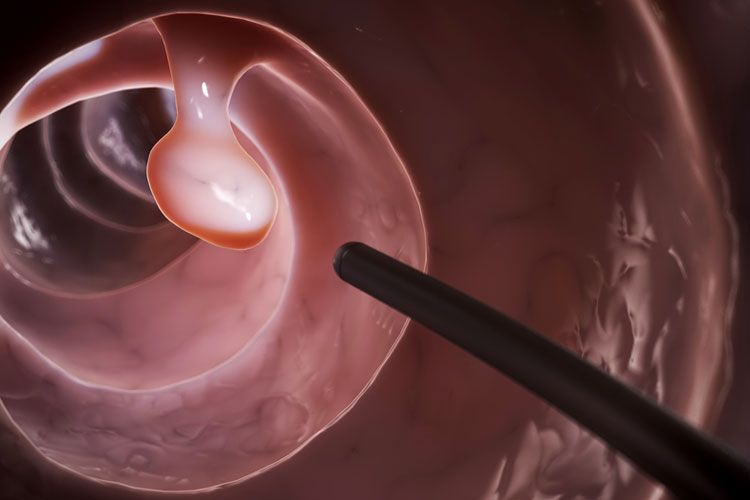
The MBS Review Taskforce has targeted alleged excesses in colonoscopies, sleep studies and diagnostic imaging for lower back pain, despite a taskforce committee on general practice having yet to begin work on specific reforms for primary care.
Attacks on “low-value” GP items grabbed the most attention when the panel’s interim report was released last week.
However, the MBS Principles and Rules Committee and six clinical committees released a raft of recommendations affecting general practice among more than 50 initial recommendations to modernise Medicare.
One committee demanded a crackdown on over-servicing for colonoscopies, noting huge disparities across regions.
“The committee is concerned that asymptomatic low-risk patients are undergoing low-value colonoscopy services for bowel cancer screening and/or too-frequent screening for a range of gastrointestinal disorders,” it said.
“The committee notes that low-value testing may be compromising access to services for patients who require clinically necessary colonoscopy services.”
Another committee noted a surge in MBS claims for assessments of obstructive sleep apnoea, saying claims for home-based studies had jumped by 160% in five years.
“While the introduction of sleep studies to the MBS has improved access to testing, there is concern that this may have led to a decrease in the quality of testing,” the thoracic medicine committee said.
In some cases, there was also a potential conflict of interest where doctors worked with clinics that sold CPAP devices to patients with low-level OSA.
Specifically, the committee recommended patients be assessed by a GP using validated assessment tools before referring for testing, and that all patients should also see a specialist before treatment was initiated.
Separately, GP requests for CT scans and X-rays for patients with lower back pain would be curbed, along with MRI requests by physiotherapists and chiropractors.
The Principles and Rules Committee said all doctors should have to pass a test on Medicare billing practices before they could receive an MBS provider number.
It said many clinicians had a limited understanding of Medicare billing rules and “may adopt questionable practices on the advice of colleagues”.
Training and testing by a government authority would mean a “modest” impost on healthcare providers, but benefits would flow from more efficient administration and a reduced risk of incurring penalties from breaches of MBS billing requirements.
It said professional colleges should include education on MBS rules and processes as part of continuing professional development programs.
On GP referrals to specialists, the committee noted an apparent excess of initial specialist and consultant physician attendances.
“In part, this may be due to confusion over whether initiation of a new referral is linked to the ability to claim an initial attendance,” it said.
It recommended clearer rules and definitions of a “single course of treatment” and time-tiered attendances for specialists and consultant physicians, as currently apply to GP attendances.
To reduce overbilling and improve transparency, it said clinicians should be limited to a maximum of claiming three MBS items for a procedure.
“It is now commonplace, for example, for many surgical procedures to be billed using different multiple item numbers for the same surgery,” it said.
“This practice is not transparent, potentially unfair and appears to be a misuse of the intention behind the multiple operation rule.”
Doctors and consumers are invited to offer their views on the recommendations in a consultation process open till 7 October.
Despite complaints from some providers and consumers, the rules committee said the three-month limit on specialist-to-specialist referrals should stay in place.
It said referrals should reflect GPs’ primacy of as gatekeepers to the health system, and the three-month time limit promoted patient-GP contact.
“This was seen to be especially important when the patient’s condition changes or they develop new conditions, and these can be better and more efficiently managed by the GP.”