Behind every policy and statistic is a real person, a real family, and a GP doing their best with limited time and support.
People often think general practice is about quick scripts and simple colds but here’s a glimpse of what an ordinary day in my rural clinic actually looks like.
I start the day by diagnosing a life-threatening neck bone fracture in a young girl who walked herself into urgent care after falling from a horse. She’s safely transferred to a neurosurgery team in Melbourne.
A kid is brought in by his worried mother for vaccination and developmental assessment. His mum is concerned he’s not engaging with his kindergarten peers. We have a long discussion about potential causes and agree on a management plan, including referral to a paediatrician for further assessment.
A young woman comes in anxious about not conceiving after nine months of trying. We spend time discussing investigations, lifestyle factors, and next steps, while I reassure her that even if infertility is a concern, there are many effective options to explore.
A teenager, brought in by his father, struggling with anxiety and cannabis use. It’s another long consult; building rapport, understanding root causes, and agreeing on a shared plan to navigate this difficult chapter together.
I’m called to admit a patient to the ward. As soon as I see the name, I recognise it – my patient whom I met after his cancer was diagnosed six months ago. He is transferred back from a tertiary hospital after his end-stage cancer was deemed incurable. As I enter the room, his wife breaks down and seeks shelter in my arms.
I finish the day with a patient I’ve known for a few months, living with multiple chronic conditions. She bursts into tears:
“I’m tired of seeing specialist after specialist, not knowing what’s the best treatment,” she says.
We have a long conversation, make shared decisions, and agree to look after her mental health alongside her physical health. She leaves with a smile that makes my long day worth all the effort.
Then comes the paperwork! Unpaid, after hours, as always.
The Health of the Nation report by the RACGP shows that 86% of GPs manage conditions non-GP specialists typically treat, mainly due to limited access or cost barriers to seeing a specialist.
Related
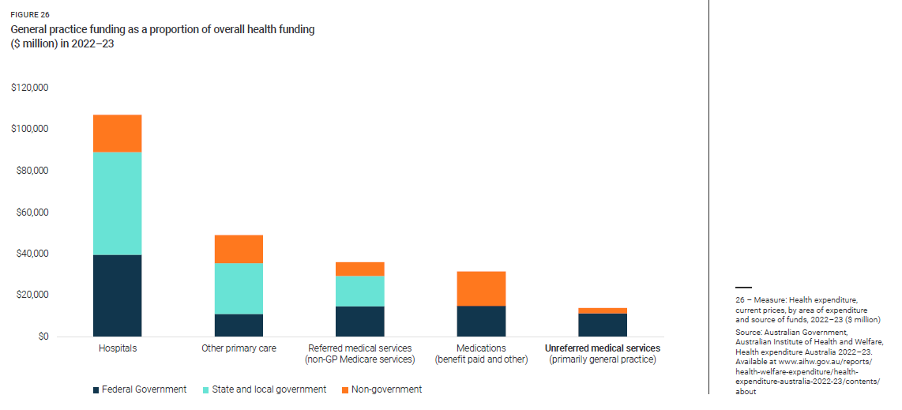
The irony? Primary care receives the lowest proportion of government funding (see image below), and to top it off, the longer the consult, the less your rebate per minute.
The recent recognition of rural generalists is a welcome step but without clarity on rebates and long-term funding, the pressures highlighted in the Health of the Nation report remain very real.
Having worked in different specialties as a prevocational trainee, I believe the nature of general practice makes it one of the most rewarding careers. The day I found that one of my young, fit, asymptomatic patients had two almost fully blocked heart vessels, picked up through timely screening, was as rewarding, if not more, than the day I did my first surgery as a surgical resident.
The difference is that prevention isn’t as visible. Our brains struggle to quantify the value of what didn’t happen (the heart attack that never came). But the evidence is clear: prevention is as important as treatment, if not more so. Yet it is too often overlooked.
I’m not asking for quick fixes or applause.
I’m asking for long-term, strategic investment that values continuity, prevention, and trust, the pillars that keep our communities well long before hospitals are needed.
Because behind every policy and statistic is a real person, a real family, and a GP doing their best with limited time and support.
We owe it to all of them to plan beyond election cycles.
Dr Tina Zafari is a GP registrar in regional Victoria, an AMC Council member representing international medical graduates and a passionate advocate for health and AI literacy. Her career has spanned clinical practice in public and private, research and community engagement.
This article was first published on Dr Zafari’s LinkedIn profile. Read the original article here.
Disclaimer: This reflection is shared to highlight the realities of rural general practice. All patient stories are fully de-identified and represent typical examples seen in everyday clinical work.





