Experts warn that a society-wide shake-up is needed, not just more resources.
The National Health and Medical Research Council has awarded $4.6 million to new research to improve youth mental health services.
But experts warn that investing in an already broken mental healthcare system could lead to even greater inefficiency.
The NHMRC, through the Partnership Project scheme, is investing in youth mental health as part of a wider $15.6m investment in 12 collaborative health and medical research projects.
The projects will also be supported by $28.6m in funding from other partners.
“The projects receiving funding under today’s announcement will inform national mental health policy and services, ensuring they meet the real-world needs of young Australians,” said Assistant Minister for Mental Health and Suicide Prevention Emma McBride.
But while investment into medical mental health research is all well and good, “mending a broken system will require much more than increasing resources”, experts have said.
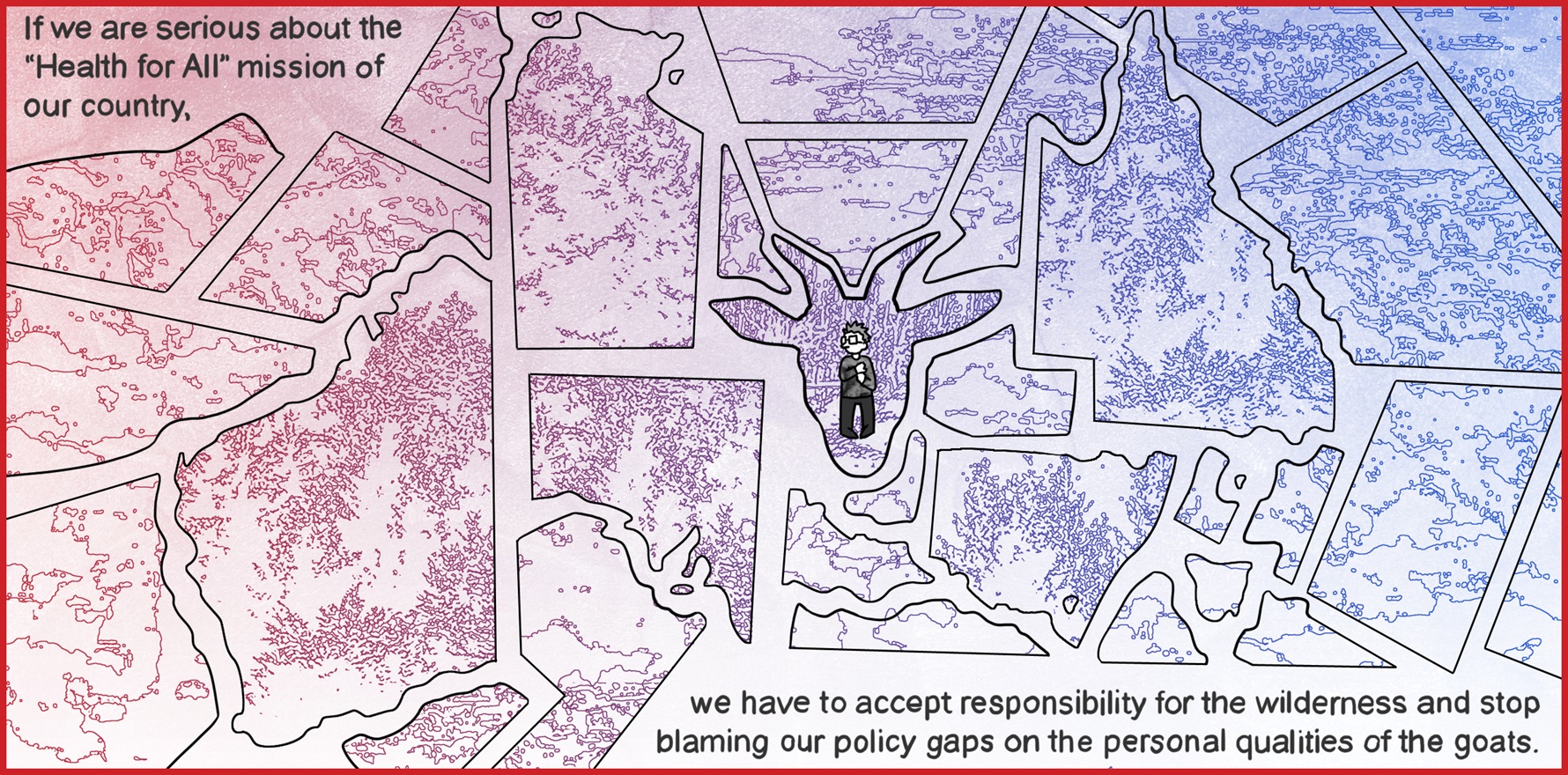
In an article published in The Medical Journal of Australia yesterday, Associate Professor Shuichi Suetani, Professor Neeraj Gill and Professor Luis Salvador‐Carulla argue that while a limited workforce and insufficient investment have often been blamed for the current mental health crisis, investing in a broken system is unlikely to solve the problem.
“To pour more investment into the existing mental health workforce without addressing the key drivers of failure can lead to even greater inefficiency,” they write, citing the work of Patel and colleagues.
“This has already been demonstrated by over 30 years of mental health plans and policies in Australia.”
According to the authors, the Global and Local Observation and Mapping of Care Levels project showed “significant gaps” in the provision of mental health care and workforce capacity in Australia, compared to parts of Europe.
“These deficiencies compound the lack of highly qualified professionals in the public mental health sector with a continuous drift of these professionals (eg, psychiatrists, nurses and psychologists) to the private sector,” they say.
Currently, the “reductionist” approach encouraged by the mental health care system, which dichotomises patients into those with and without a mental health disorder diagnosis, “puts disproportional emphasis on specialists over generalists, medication over psychosocial support, and hospital care over community care despite no evidence that a higher density of mental health professionals reduces the prevalence of mental disorders”.
“Even though social determinants of health and social justice issues are often the root causes of many mental health difficulties, little complementary efforts are made to address these in the current system.”
As such, mental health care warrants a total redesign, shifting towards a “biopsychosocial framework” that invests widely in a “whole of society” preventative approach, not just the traditional mental health workforce.
“Better integration of acute and community care as well as mental health and drug and alcohol care systems is urgently needed.
“We also need to address the socio‐economic and structural determinants of mental health and focus on the antecedents and consequences of mental health difficulties.”
Related
The authors say more care should be provided in the primary sector.
“In terms of the psychiatry workforce, more training needs to be provided to care for people with mental health difficulties in primary health settings.
“For this, psychiatry trainees should have more training positions and experience in GP liaison settings where they have exposure to high prevalence mental disorders in a supervised environment while building relationships with primary health colleagues.”
But care should extend beyond general practice and specialist clinics.
“We must be able to provide psychosocial interventions in settings beyond GP surgeries and mental health clinics.
“Without such fundamental transformation, we cannot mend the broken system.”
Further details on the NHMRC projects receiving funding can be found here.