New US research suggests antibiotics have ‘no measurable impact’ on cough duration or severity in acute LRTIs.
Simple symptom-relieving medications, patience and not antibiotics are best for relieving cough, new research suggests.
Most lower respiratory tract infections – which lead to coughing – are caused by viruses, meaning antibiotics will have no effect. A recent prospective, observational study, published in the Journal of General Internal Medicine, confirms antibiotics do not reduce the severity or duration of cough in acute LRTIs.
Researchers recruited over 700 adults from primary and urgent care clinics across three US cities presenting with a cough up to two weeks duration and at least one of the following symptoms: shortness of breath, sputum or phlegm production, body/muscle aches, chest congestion, chest discomfort when coughing and a fever (or reports of feeling feverish, chills or sweats). All patients would be diagnosed with a LRTI.
Of these, 29% received at least one antibiotic (most commonly amoxicillin-clavulanate, azithromycin or doxycycline) while just 7% received an antiviral (oseltamivir or nirmatrelvir-ritonavir).
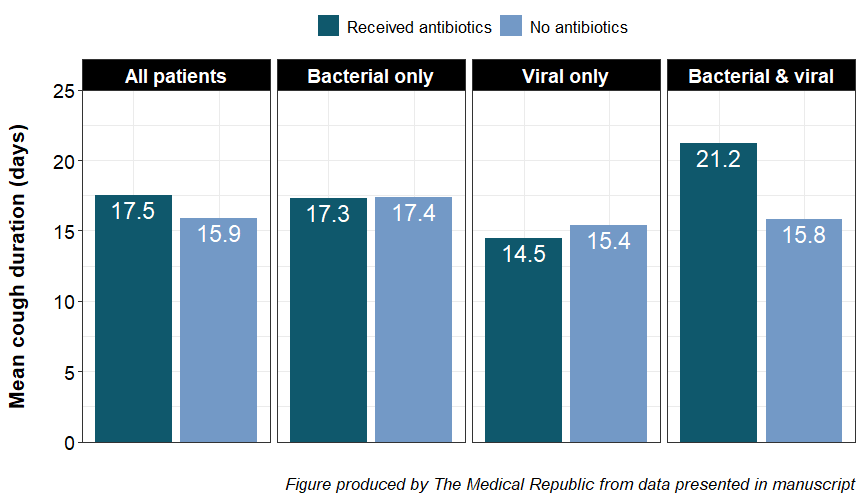
Receiving antibiotics did not reduce the average cough duration when all patients were considered. There was also no effect of antibiotics on cough duration in patients who only had a bacterial infection, nor was there a difference in patients with just a viral infection. However, antibiotics increased cough duration in patients with both a bacterial and viral infection.
“We know patients have unrealistic expectations about [the] duration of cough and expect that receiving antibiotics will reduce the duration of their illness,” said Dr Kerry Hancock, chair of the RACGP’s respiratory medicine specific interest group.
“However, on the basis of this study (and others), GPs can be confident in explaining to patients that, on average, cough will last over two weeks regardless of the pathogen and whether antibiotics are prescribed.”
Related
Patients who received antibiotics had a more severe cough (mean Bronchitis Severity Score 7.6 versus 6.8; range 0-15) and had been dealing with their cough for longer (average duration 6.2 versus 4.7 days) prior to presenting compared to patients who did not receive antibiotics.
“Clinicians prescribed antibiotics when they felt patients were sicker,” the researchers concluded.
“Prescribing antibiotics for infections where patients are unlikely to benefit ‘medicalises’ that illness and makes it more likely that they will seek care and an antibiotic with subsequent infections.
“This is important for public health authorities as it demonstrates where clinician education may be necessary and important to decrease unnecessary antibiotic use.”