Productivity Commission data puts GP-type emergency presentations at record lows.
As health minister Mark Butler edges ever closer to opening his government’s promised 137 urgent care clinics, one may be forgiven for questioning their worth.
The interim evaluation of the clinic model is now almost one year old, and the Department of Health, Disability and Ageing website simply gives the expected delivery date for the final evaluation report as “2026”.
As a refresher, that interim evaluation found that each UCC presentation cost the commonwealth about $216 and that the 63 clinics with data available at the time could prevent up to 334,000 emergency department presentations annually.
The interim evaluation noted that this estimate relied on the accuracy of the UCC reporting when it came to answering the question “where would the patient have gone otherwise”.
“This may under or over-estimate the level of ED attendances avoided due to the data limitations … future evaluation reports will have access to data across a full year of operation for Medicare UCCs and be able to triangulate these estimates with additional causal analysis using ED data,” the report reads.
“Additionally, the analysis will be extended to include an assessment of the cost impact for presentations in which it is indicated the patient would have taken actions other than attending an ED or calling an ambulance.”
In lieu of an extended analysis, however, the annual Productivity Commission Report on Government Services (ROGS) does collect information on presentations at public hospital emergency departments.
According to the 2026 ROGS report, which was released on Friday, potentially avoidable or “GP-type” presentations to public hospital emergency departments hit a 10-year low in 2025.
Related
While a somewhat crude measure, the number of GP-type ED presentations initially increased year-on-year since the Productivity Commission started collecting data in 2015, reaching a height of 3.2 million in the 2020-21 financial year.
It dropped back to just over 3 million the following year, before falling more dramatically to 2.8 million in 2022-23.
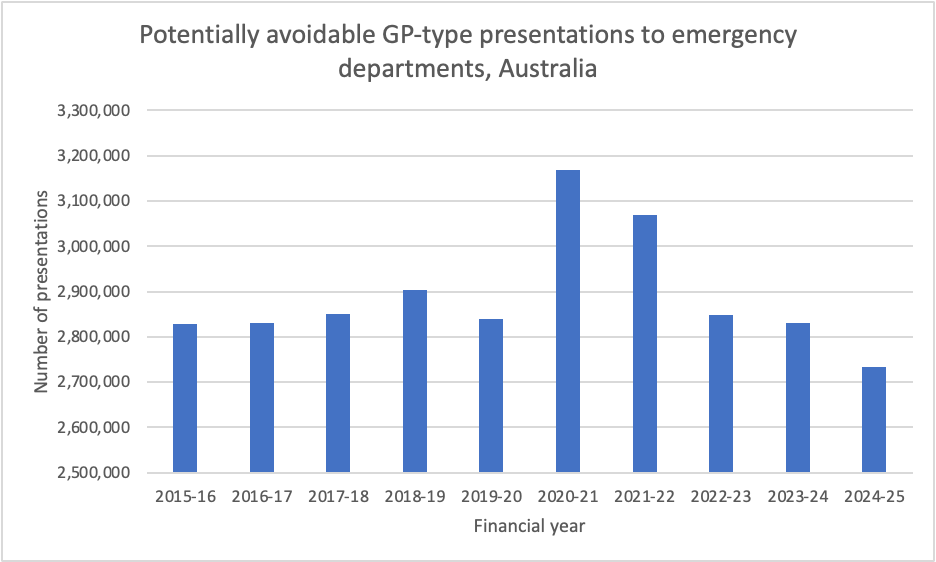
The first Medicare urgent care clinics didn’t open until June of 2023, the beginning of the 2023-24 financial year; the dramatic drop in GP-type hospital emergency presentations predates the opening of the UCCs.
GP-type attendances for 2022-23 (i.e., the year right before UCCs went live) and 2023-24 (the year right after UCCs went live) remained relatively stable in terms of raw numbers.
Between the 2023-24 financial year and the 2024-25 financial year, the number of GP-type presentations to emergency dropped by approximately 100,000.
The number of presentations for 2024-25 was lower than it ever was pre-pandemic and before the introduction of UCCs.
The question of whether UCCs are or are not working as intended, therefore, remains unanswered.
It should also be noted that, while UCCs are advertised under the Medicare banner and services are technically bulk billed, there are certain exemptions in place which make UCC bulk billing different to GP bulk billing.
The major difference is that UCCs are exempt from section 19(2) of the Health Insurance Act 1973, which forbids a clinician from receiving any additional compensation for a bulk billed service.
This allows UCCs to receive government grant funding in addition to bulk billing.