Electronic health records have brought efficiencies to the medical note while introducing new challenges
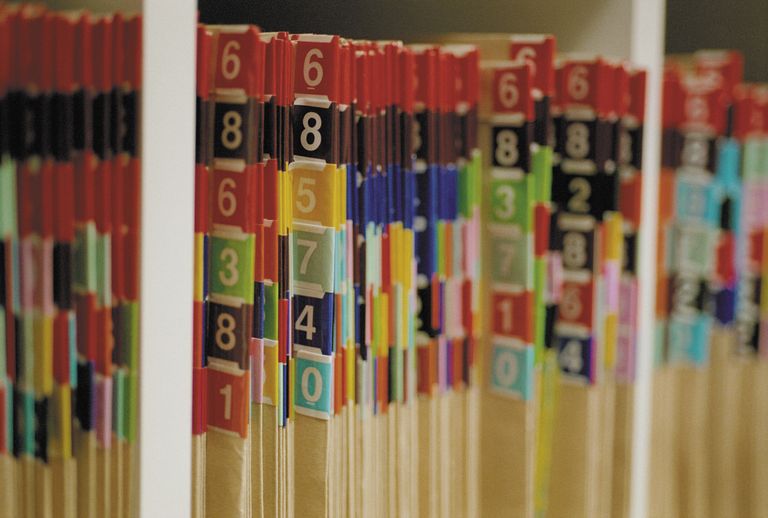
There was a time when documentation was an almost inconsequential process. After seeing a patient, the doctor would scratch a note, close the folder, and file it on a shelf until the next visit.
Things are different and the medical note has evolved. As it’s evolved, electronic health records (EHR) have brought efficiencies to the medical note while introducing new challenges. And like the cognitive biases that impact patient care, the problems inherent in documentation need attention.
Thinking about these challenges becomes important in documenting care and training the next generation of health professionals. Here are a few that I think about
Auto documentation
One of the powers of the EHR is that it allows users to auto-populate the medical record with chunks of pre-fabricated text known as smart phrases. But these personally created building blocks of the medical note create the potential for one-clip-fits-all documentation. As I’ve said in the past, the smart phrase is not new technology.
I work to keep smart phrases out of my history of present illness and impression where individualized narratives show what’s unique about a case. Free text keeps me real.
Replicability
While smart phrases represent the dropping of self-created language, we have the ability to clip and paste information from other parts of the chart. This may include bits and pieces from notes penned by another medical professional.
While we all lift bits of language from places like CT and biopsy reports, issues arise when the origination of our language is that of another health professional. Epic now allows visualization of a phrase’s origin when not created by the author.
I’m careful about what I copy. I’m twice as careful with what I paste as representation of my own thinking.
Size and absence of constraint
While smart phrases are limited only by our imagination, a digital note with no constraints predisposes to note bloat, one of the looming threats to modern medicine. Pre-digital notes were constrained by writer’s cramp.
I’ve labored through notes where every single lab drawn on a complicated patient is dumped into the note. Pages and pages of marginally abnormal CBCs and metabolic panels create a scenario where it’s difficult, if not impossible, to discern what data is relevant to the decisions made.
I try to consider the needs of the end user of the note. Of course, this is challenging when our opinion of what constitutes a ‘good note’ varies from that of the note reader.
Ambiguity of purpose
To me this is the most remarkable phenomenon of the modern medical note note.
Medical notes have traditionally had pet purposes. Medical students learn early on that ‘the write way to write a note’ varies not only by specialty but by the whim of the individual physician responsible for the note. Physicians with firm views regarding what constitutes the purpose of a note may even morph their perspective depending upon the nature of an individual case.
So if you ask three physicians the purpose of a medical note and you’ll get five answers ranging from billing and quality documentation to legal coverage and professional communication. Over time the medical note has morphed into all of these things at once.
The problem with ambiguity of purpose is how to manage the expectations of the end user. A physician who feels compelled to paste three months worth of blood results into the data portion of a note will be at odds with someone like myself who believes that a note serves to offer nothing other than concise support for what I’m thinking and planning.
As notes become more visible to more folks we can expect ambiguity of purpose to become more pronounced. Digital notes and their capacity for customization amplify this divergence of purpose.
Scaling visibility of the EHR
Once restricted to the shelves of offices in big buildings, medical documentation has traditionally been silo’d. This was fine because notes existed for the doctors who occupied those individual offices. The medical note is now enjoying new freedom in its electronic shape. More notes are more visible to more professionals. This is evident within consolidated health systems where networks of offices connect to big hospitals.
Beyond professionals, patients are watching and, in some cases, editing their own notes. OpenNotes is a related program based in Boston’s Beth Israel hospital. Regular patient review and revision represents a revolutionary move in medical documentation.
This scaling visibility of the modern note brings greater scrutiny for what we do or don’t do.
This idea of the medical note and its evolution gets little attention yet it represents the core medium of all documentation by medical professionals. It deserves more thorough attention and study.
Dr Bryan Vartabedian is a US-based gastroenterologist.
This blog was originally published on 33charts.