The vasodilatory effects may prove beneficial upstairs as well as downstairs.
A recent study proposes a potential new therapy for Alzheimer’s – the (in)famous little blue pills.
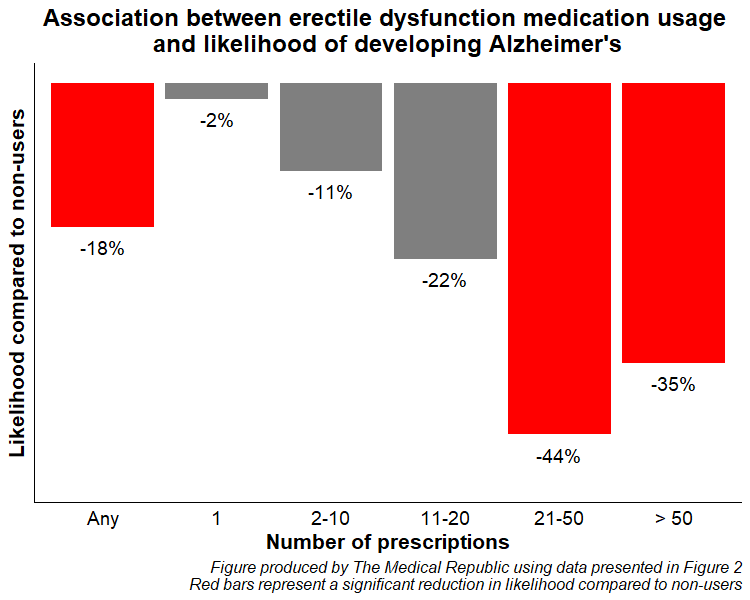
Men taking erectile dysfunction medication are 18% less likely to develop Alzheimer’s compared to men who don’t, new research published in Neurology suggests.
As part of the UK-based population cohort study, researchers looked at 270,000 men aged 40 years and older who had been newly diagnosed with erectile dysfunction.
After following these men for a median duration of five years, approximately 1000 participants developed Alzheimer’s, with a greater crude incidence in those not taking vitamin V (9.7/10,000 person years) compared to those who were taking erectile dysfunction medication (8.1/10,000 person years).
Compared to non-users, erectile dysfunction medication use (sildenafil, tadalafil or vardenafil) was associated with an 18% reduction in the likelihood of developing Alzheimer’s disease, after controlling for factors such as age, smoking, alcohol intake, BMI, socioeconomic deprivation and comorbidities such as hypertension, depression and a history of head injury.
The apparent protective effect increased in those with a greater number of erectile dysfunction medication prescriptions.
“[Phosphodiesterase type-5] enzyme inhibition could play a role in modulating vasodilatory responses in the CNS,” wrote the authors of an accompanying editorial.
“Additional mechanisms by which PDE5 inhibitors could improve brain health and reduce the risk of [Alzheimer’s] include increasing cerebral perfusion and reducing neuronal metabolic demands.”
Related
Alzheimer’s disease is the most common form of dementia worldwide, with limited effective treatments and no known cure. Erectile dysfunction drugs such as sildenafil are often repurposed as therapies for other causes, including pulmonary arterial hypertension. Some evidence suggests the enzyme phosphodiesterase type-5 is elevated in Alzheimer’s patients but, to date there had been no consensus on whether PDE5 inhibitors are protective against dementia.
Researchers felt the ability of ED medications to cross the blood-brain barrier contributed to their protective effects, and the apparent dose-response relationship.
“The availability of these drugs in the CNS where they can exert their inhibitory effect on [phosphodiesterase type-5] in brain cells may be suggestive of the mechanism that contributes to some level of neuroprotection,” they wrote.
“The protective effect we observed from the increasing cumulative number of prescriptions may also suggest that repeated exposure can lead to greater accumulation of PDE5I in the brain.”
Subgroup analyses revealed individuals who were prescribed sildenafil had a 19% reduction in the likelihood of developing AD compared to non-users, but no such associations existed for those prescribed tadalafil and vardenafil.
Similarly, a lower risk of Alzheimer’s was found in older ED drug users (24% reduction in patients 70 years and older, no association in patients under 70 years) and those with diabetes (29% reduction in patients with diabetes, no association in those without diabetes) compared to non-users.
A key limitation of the study is that researchers only looked at prescriptions for ED medications, not whether the men filled the prescriptions or took the pills.