Vaping could be a very effective tool for reducing smoking in Australia, but our restrictive laws have ensured a black market of dubious products.
Smoking is still Australia’s leading preventable cause of death and illness. GPs in Australia see over 80% of the population every year, and are well placed to help smokers quit.
But as GPs know, conventional smoking cessation aids are not very effective and quit rates are low.
Also, GPs are very busy and few are comfortable trying to be a quit smoking coach. In addition, few smokers seek help as they think smoking is a lifestyle issue rather than a disease to be treated by a doctor. So, the GP contribution to reducing smoking in Australia has been modest.
Efforts to reduce harm from smoking changed forever in 2007 when the first generation of nicotine vaping devices entered the market. It took a few years before vaping took off. Now an estimated 82 million people in dozens of countries around the world are vaping. Vaping is also the most popular quitting aid in Australia and around 1.1 million adult Australians vape.
Nicotine vaping devices are used as a short-term quitting aid or as a long-term safer alternative to smoking. Vaping is significantly more effective as a quitting aid than nicotine replacement therapy, according to a Cochrane review published in November last year.
Vapes deliver the nicotine smokers crave but without the combustion, smoke or tar and with only a small fraction of the chemicals in cigarette smoke. Nicotine itself can cause dependence but is otherwise relatively benign. It does not cause cancer or lung disease and has only a minor role in cardiovascular disease.
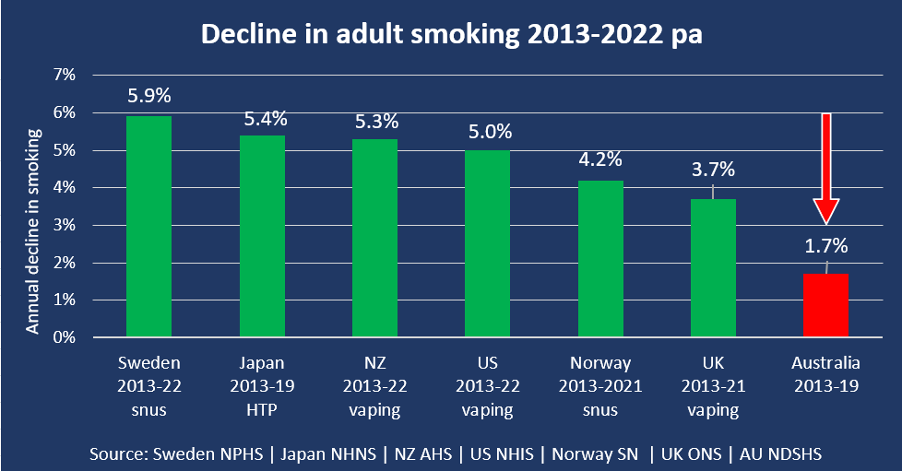
The decline in smoking rates accelerated in the UK, US and New Zealand after nicotine vaping became widely available. In New Zealand, after vaping was legalised in August 2020, the adult smoking rate fell by an unprecedented 33% in two years from 2020-22.
However, Australia’s hostile position on vaping has resulted in lower vaping rates, and a slower decline in smoking than in many other comparable countries such as the UK, US and New Zealand (vaping). Other forms of tobacco harm reduction have also proved to be effective in reducing smoking rates in Japan (heated tobacco products), Sweden and Norway (snus – an oral smokeless tobacco product).
Since 1 October 2021, Australians have required a doctor’s prescription to purchase nicotine liquid from a pharmacy or to it import from overseas. However, difficulties obtaining nicotine liquid legally appear to have resulted in a spectacular increase in the black-market supply. As is typical of black markets, there is no quality control or restriction of sales to children or youth. But the inferior quality of some vaping devices and the ready access of vaping to youth has been blamed on vaping rather than the unrealistically severe restrictions imposed by Australian government policy.
Australian GPs should try to identify as many patients as they can who smoke, explain that smoking-related diseases account for two out every three deaths of long-term smokers, and that help with quitting is readily available from Quitline and other services.
Vaping is an approved second-line quitting aid for smokers who are unable or unwilling to quit smoking. It is also the most popular quit smoking aid in Australia. There has not been a documented death globally from nicotine vaping in 15 years.
Staff at vaping shops are generally former smokers who managed to quit by switching to vaping. Not only are they extremely knowledgeable about vaping but they are also highly motivated to assist their customers to succeed in quitting by vaping.
The fierce resistance to nicotine vaping in Australia and the accompanying barrage of misinformation may seem inexplicable. But new drug harm reduction interventions are usually resisted long after evidence of effectiveness and safety is clear. Eventually new drug harm reduction interventions are usually accepted and, after a delay, deployed to scale. This is also likely to happen with vaping in Australia.
Smoking is present across the social and economic spectrum. But low-income and disadvantaged populations have higher smoking rates, smoke more cigarettes per day and have more difficulty quitting. Lower smoking rates will also reduce health and financial inequalities.
The world now has the means to rapidly accelerate the end of smoking, the cause of eight million deaths worldwide every year. Most smokers want to quit but find quitting very difficult. Some tobacco companies also want to quickly transition away from combustible cigarettes to a range of non-combustible products.
But amazingly, tobacco control and public health in Australia and some other countries are working overtime to minimise the number of smokers switching to vaping even though vaping is at least 95% less risky than smoking.
After the devastating impact of covid on health in Australia, GPs now have an opportunity to encourage their patients who still smoke to quit by switching to vaping.
The NSW Greens have recently announced their support for revising the regulation of vaping to minimise the black market and ensure the availability of nicotine vaping for adult smokers while restricting the availability off vaping for youth. This requires ending prescription control of nicotine for vaping which has failed abjectly.
However, there are a number of steps that would be required before the Greens proposals become policy. The vaping issue has entered a new phase. As has happened so often before when new drug harm reduction interventions are being considered, ferocious resistance has delayed the widespread use of a very effective tool for reducing the huge toll of smoking in Australia.
Dr Alex Wodak AM is an emeritus consultant at the Alcohol and Drug Service, St Vincents Hospital, Sydney.







