Similar approaches to those used in covid vaccines may have potential for analgesia.
Nanoparticle-based therapeutics are commonly used in cancer patients, but there is growing evidence to suggest they could also be used to improve treatment options for chronic pain.
Speaking to delegates at the annual scientific meeting of the Australian Pain Society in Darwin last month, Dr Nicholas Veldhuis, researcher at Monash University, said new biology has been discovered simply by working with nanomaterials, and this might soon be put to work developing new therapeutic options for pain.
“We’re all familiar with the idea that it’s incredibly challenging to get drugs through the planning [and] preclinical phase all the way through to market entry,” he said. “This is no different for analgesics, but you would argue it’s a much harder battle for analgesics.
“[Pharmaceutical companies currently] don’t invest a lot in analgesic drug delivery, compared to what they used to. Everyone’s running scared, especially in terms of moving away from opioids.”
Some of the barriers and challenges in translating drugs from benchtop to bedside include unwanted toxicity (leading to potentially severe side effects), targeting the right receptors in the right tissue and instability or rapid clearance (where the drug metabolises and is passed by the body before it gets the opportunity to exert its desired effect).
This led Dr Veldhuis and his team to consider whether they could employ some of the advances in drug delivery approaches to overcome some of these limitations.
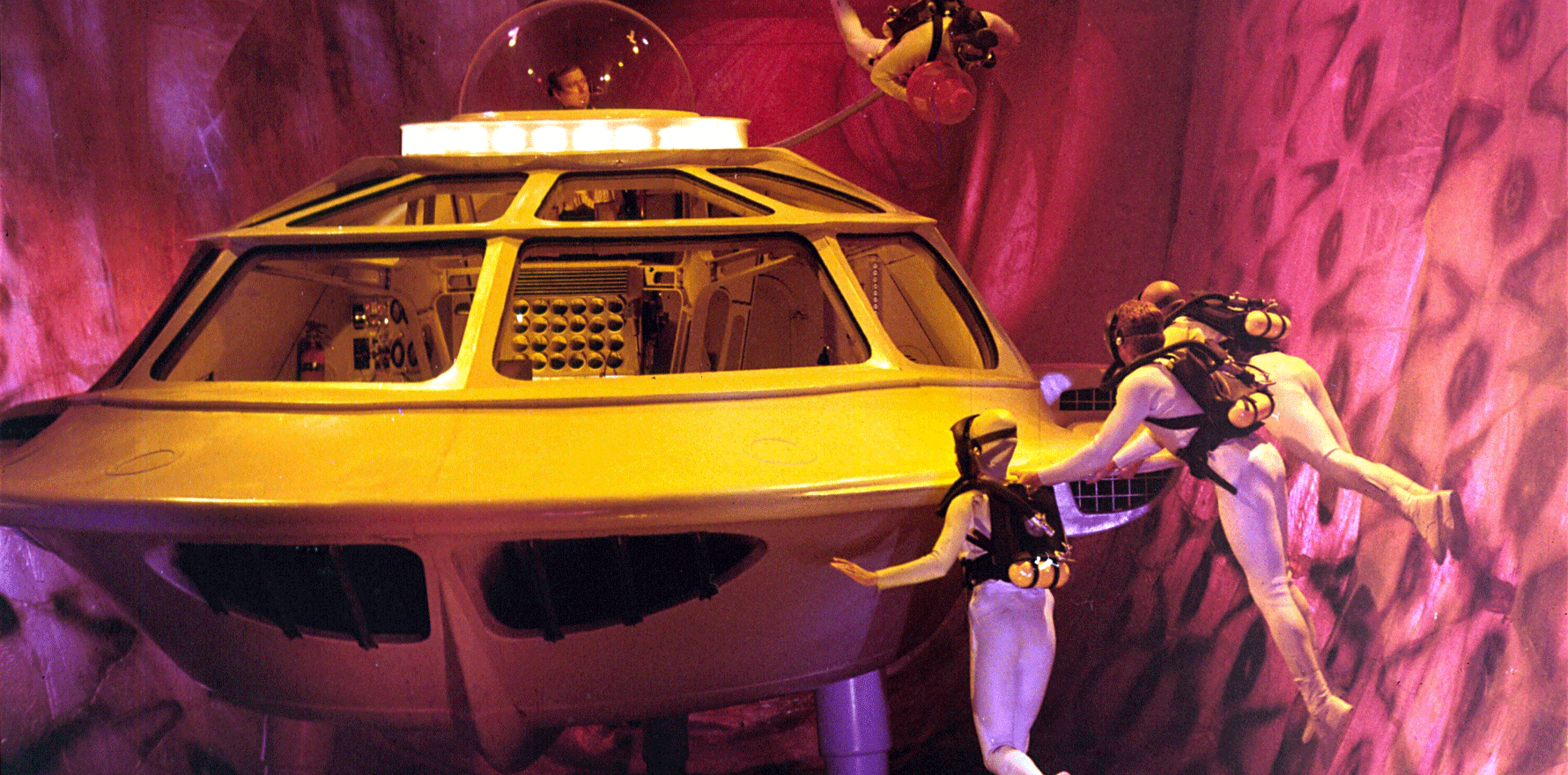
One particularly neat improvement in how drugs are delivered has been the use of lipid nanoparticles in mRNA vaccines. Over 50 million doses of mRNA vaccines have been delivered in Australia since the covid pandemic began.
“Now people like my mum talk about RNA and mRNA delivery,” said Dr Veldhuis. “I could not have imagined that five years ago. She never would have said anything about RNA, or a lipid nanoparticle. But it’s part of the vernacular now.”
The lipid nanoparticles help stabilise the vaccines and allow for a controlled release of a small amount of RNA to elicit an immune response.
Related
Dr Veldhuis has used a similar controlled release approach using lipid nanoparticles to improve analgesic drug delivery, designing a system where aprepitant (Emend), a medication used to prevent nausea and vomiting in cancer and postoperative patients, is embedded in pH-responsive nanoparticles.
Aprepitant is an antagonist of the neurokinin-1 (NK1) receptor, which moves from the plasma membrane of cells into acidified endosomes – rather than simply sitting at the cell surface – to maintain the transmission of pain signals.
The pH-responsive nanoparticles are also taken into the endosome, where the aprepitant is released and can act on the NK1 receptors, preventing the substance P-induced activation of the NK1 receptor and therefore stopping pain transmission.
“The [nano]particle [delivery system] doubled the efficacy and duration of pain relief,” Dr Veldhuis explained.
Much time and money has been spent trying to target the NK1 receptor, but aprepitant has been the only real reward for effort. Dr Veldhuis feels the lack of success is partly due to a failure to appreciate that receptors don’t always stay in the cell membrane but can be internalised during pain signalling.
“Some of the pitfalls may be related to the research and development that’s been done [when] NK1 is at the cell surface. We think a lot of the drug discovery was focusing here.… [Our] research is teaching us a lot about how nanomaterials can be exploited to move drugs to different places and change outputs.”
It’s still early days for this line of research, with human trials still to come, but Dr Veldhuis is confident more targeted approaches, like the use of nanoparticles, could help speed up the development of effective, long-lasting and non-opioid treatments for chronic pain.