Cancer patients may be at greater risk of dying from COVID-19, particularly those with lymphomas, leukaemias or myelomas, according to two studies from China and the United States
Happy Monday from The Medical Republic‘s live COVID-19 blog.
Thanks for joining us, and thank you to our sponsor and supporter for funding this project with an independent grant, Boehringer Ingelheim.
The latest
- Current cancer patients show higher mortality from COVID-19, particularly with haematological malignancies.
- Loss of sense of smell without blocked nose is highly specific to COVID-19, study suggests.
- WHO releases latest definition of death from COVID-19 and the ABS advises on how to certify a COVID-19 death
- Cancer patients may be at greater risk of dying from COVID-19, particularly those with lymphomas, leukaemias or myelomas, according to two studies from China and the United States.
The first, published on the non-peer-reviewed preprint server MedRxiv, retrospectively looked at outcomes in 283 COVID-19 patients with cancer admitted to 33 hospitals across Hubei province in China. Just over one quarter of patients were former cancer patients who had undergone resection more than five years ago without relapse, and three-quarters were current cancer patients, around half of whom had advanced disease.
The study found that current cancer patients were more likely to have severe COVID-19 symptoms on admission. The overall mortality rate during hospitalisation was 18%, with 3 deaths (1%) not due to COVID-19. Current cancer patients also had 2.45-times higher risk of death than former cancer patients, with mortality rates of 21% compared to 9%.
The worst outcomes were seen in patients with current lymphohematopoietic malignancies such as lymphoma and leukaemia, and all seven patients with these malignancies who had recently undergone chemotherapy died from COVID-19.
A second study, published in Cancer Discovery, looked at outcomes in 218 patients with COVID-19 and a diagnosis of cancer who presented to New York hospitals. Three-quarters had solid tumours, and one-quarter had haematological malignancies.
This study found an overall mortality rate of 25% among patients with solid tumours, but higher in patients with lung, gastrointestinal and gynaecological cancers and lower in patients with breast and genitourinary cancers.
Among patients with haematological cancers, the mortality rate was 37%, with a trend towards higher mortality in patients with myelomas compared to lymphomas.
“Case fatality rates were 2-3 times the age-specific percentages seen in our non-cancer population and the greater New York City area for all COVID-19 patients,” the authors wrote.
Commenting on the higher mortality rate among patients with haematological malignancies, the authors said these patients were often severely immunocompromised and being treated with immunosuppressive therapies.
The other observation was that many of the patients were exposed COVID-19 through the healthcare system, before there was widespread knowledge of and response to the pandemic.
- The loss of a sense of smell is highly associated with COVID-19 infection and doesn’t appear to be linked to having a blocked nose, new research suggests.
In a paper published on the non-peer-reviewed preprint server MedRxiv, researchers report the outcomes of a cohort study in 500 patients who presented to a COVID-19 testing with acute respiratory infection symptoms.
Overall, 69 patients reported olfactory loss, and 22 of these tested positive for COVID-19. Among the 431 patients without olfactory loss, only 12 tested positive for COVID-19, so the frequency of olfactory loss in COVID-19 was 64.7%. People with olfactory loss who did not have COVID-19 were significantly more likely to have a blocked nose.
When the authors controlled for blocked nose, they found that the presence of olfactory loss had a 97% specificity for COVID-19, a positive predictive value (how many people it correctly diagnoses as having the disease) of 63% and a negative predictive value (how many people it correctly rules out of having the disease) of 97%.
“Thus, considering the high frequency of smell loss in non-hospitalised COVID-19 patients, acute olfactory impairment should be included in the WHO symptoms list and should be recognised as an early symptom of the disease,” the authors wrote.
- Meanwhile, the Australian Bureau of Statistics advises that in the event of a death from COVID-19, ‘COVID-19’ or ‘Coronavirus Disease 2019’ should be certified on the death certificate. They stress that the term ‘coronavirus’ should not be used in place of either of these. The WHO has issued emergency code U07.1 COVID-19, which should be assigned to all mentions of COVID19 on the death certificate.
The ABS says that COVID-19 should be recorded in Part 1 of the Medical Certificate of Cause of Death, and all conditions and symptoms in the causal pathway leading to death should be included. For example, if COVID-19 has caused pneumonia and fatal respiratory distress, this should be recorded alongside COVID-19 in Part 1 with as much detail as possible on the duration of each disease and symptom.
If the patient also had existing conditions that may have contributed to their death from COVID-19 – for example, coronary artery disease, cancer, or COPD – this information should be certified in Part II of the certificate. The ABS has published examples of COVID-19 certificates to help doctors with this step.
- How exactly do we define a death from COVID-19? There is an important, particularly with high mortality rates in individuals with pre-existing comorbidities such as hypertension and cardiovascular disease, and the emergence of stroke as a cause of death among individuals with COVID-19.
The WHO has officially defined what a COVID-19 death is, for surveillance purposes: “a clinically compatible illness in a probable or confirmed COVID-19 case, unless there is a clear alternative cause of death that cannot be related to COVID disease (e.g. trauma).” They also stress that for a death to be attributed to COVID-19, there should be no period of complete recovery between illness or death.
- Melbourne’s Royal Children’s Hospital is now delivering around 70% of its specialist appointments by telehealth, according to Victoria’s Minister for Health Jenny Mikakos.
The hospital normally has an average of 1200 face-to-face appointments every week day, but with the new telehealth regimen, that has dropped to around 250 a day. The number of telehealth consultations has jumped from 231 in April last year to more than 11,200 in April this year. The hospital’s IT system is using techniques like split-screens during video consultations to allow patients to view their scans.
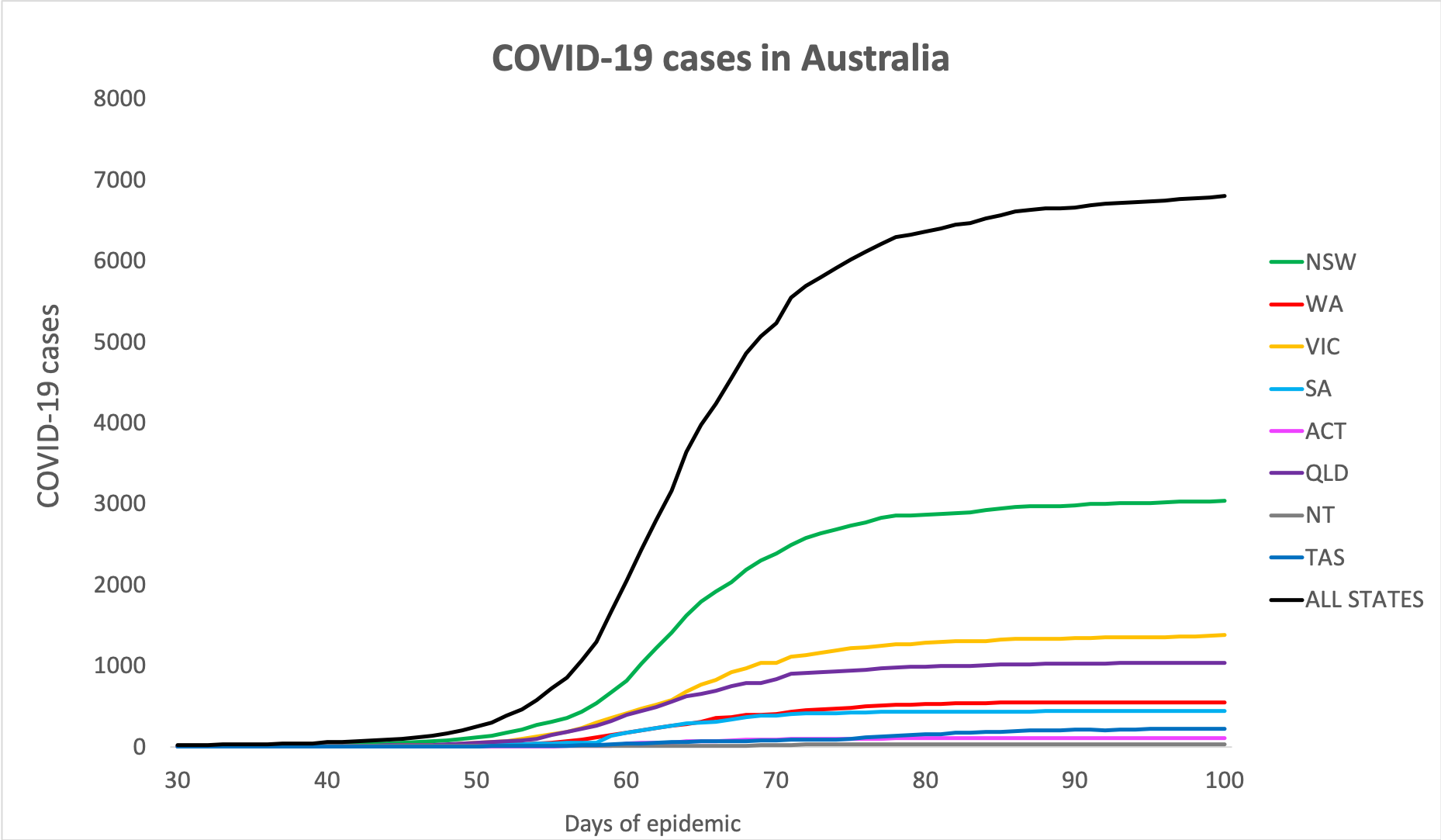
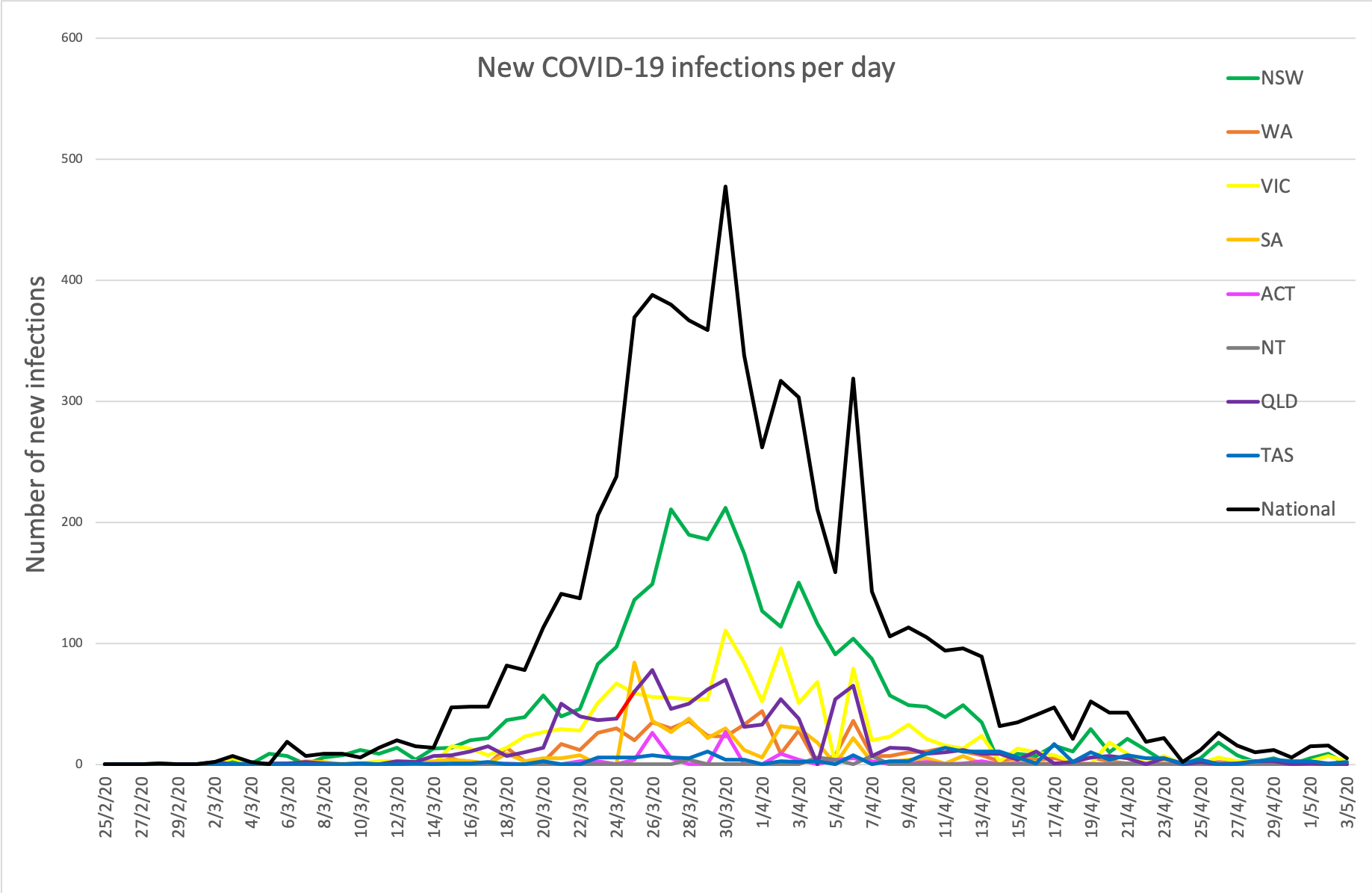
- We’ll be watching Australia’s COVID-19 infection rates very carefully over the next week to see how the loosening of social restrictions and the return to school impacts them. Fingers crossed the curve stays flatter than Dan Tehan’s mood right now.
Here are the national figures on confirmed COVID-19 infections around Australia to 9am last night:
National – 6801 (up 20 since yesterday) with 95 deaths and 5817 listed as recovered
ACT – 106
NSW – 3035
NT – 29
QLD – 1035
SA – 438
TAS – 223
VIC – 1384
WA – 551
Disclaimer: The content on the Medical Republic COVID-19 blog is independently created by Medical Republic without input from Boehringer Ingelheim Pty Ltd. The views, information, or opinions expressed on the Medical Republic COVID-19 blog are Medical Republic’s own and do not necessarily represent those of Boehringer Ingelheim Pty Ltd. Boehringer Ingelheim Pty Ltd is not responsible for and does not verify the accuracy of any content on the Medical Republic COVID-19 blog.


