When Ged Kearney talks about the harms associated with defining the average patient as a white male, her government is doing the same with their modelling for GPs.
minister for health Mark Butler’s assertion that GPs will be “better off” under their new Medicare structure.
The central claim is that, according to calculations made using the General Practice Registrars Australia GP earnings calculator, metropolitan GPs who bulk bill all patients will go from making around $465,018 in billings per year to making $576,864 in billings per year.
I wish.
Underpinning the modelling are certain assumptions, including the number of people seen per hour, the amount of on-call done, the location of the practice, and the percentage paid in practice costs. I was unable to find the exact figures for each, so I’ve done the following model which seems to be roughly in line with the Minister’s proposition.
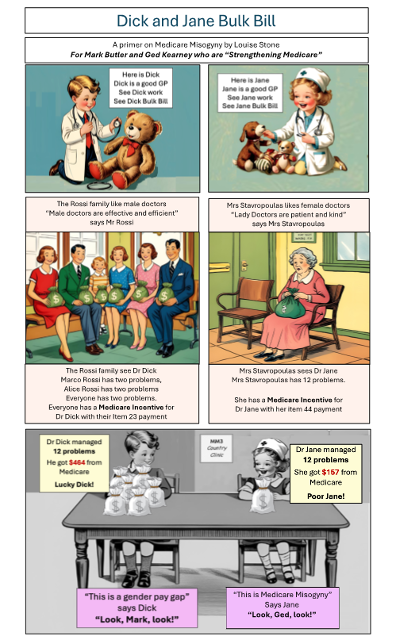
So, let’s look at Dr Dick. I’ll exclude his after-hours paperwork, which is probably around eight hours a week, for the sake of argument.
The Minister and his team have access to Medicare data in a way I don’t, so I have not included a mix of item numbers.
I’ve assumed Dr Dick is working 40 hours a week with four patients an hour and consistently charging an item 23. I’ve excluded care plans, procedures and other lucrative items, which is probably why Dr Dick is earning less than we would expect on the Minister’s calculations.
My results approximate what the Minister has found, so I think this is appropriate.
I’ve also taken the Minister’s rate of roughly $97 for a private consultation, with 53% being concessional patients who are bulk billed 90% of the time, around 50% being bulk billed. I’ve added the new “bonus” for a practice that exclusively bulk bills – “practices participating in the Program will receive an additional 12.5% incentive payment on every $1 of MBS benefit earned from eligible services, split between the GP and the practice”.
I think this means that Dr Dick gets an extra 6.25%.
I’m sure cleverer heads than mine can add in the complexity of other item numbers, but if we keep it to the most commonly used consultation numbers, here is what Dr Dick will earn.
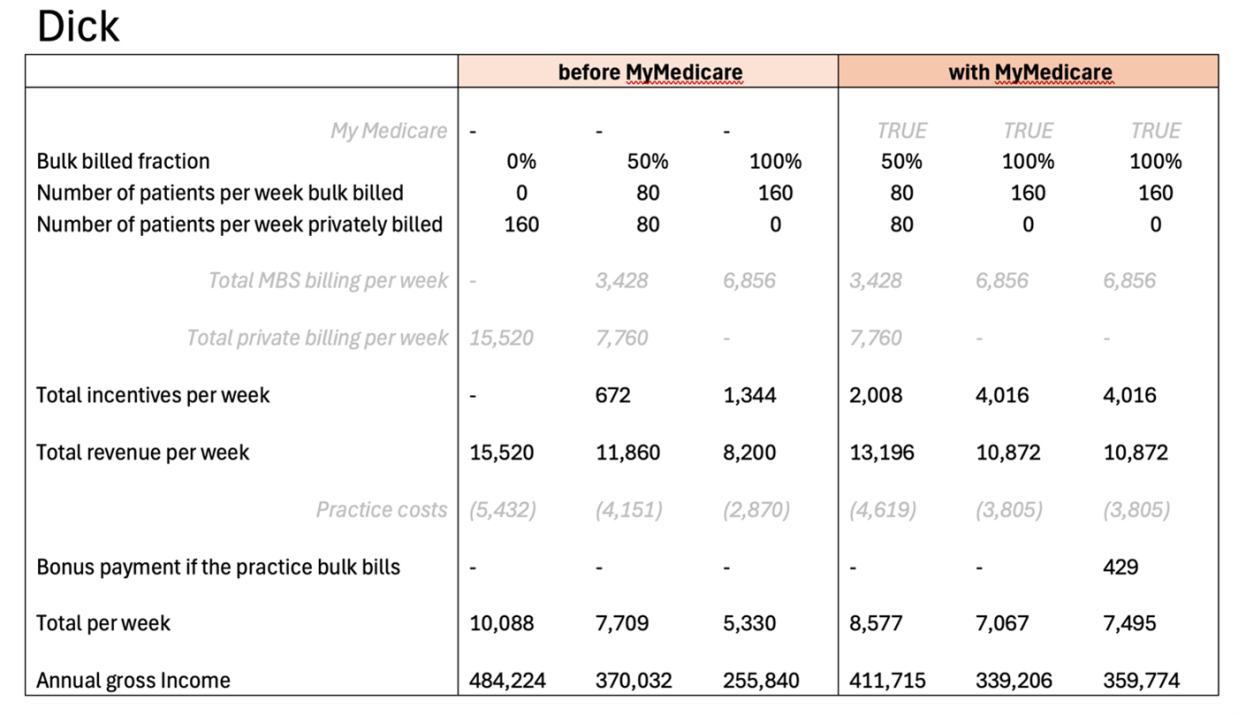
Lucky Dick is doing rather well, and will do better under My Medicare.
However, the Minister makes an assumption here. It’s a common one, but it’s unfortunate.
The assumption is that the “average” GP is the one that matters. He assumes that as long as the “average” GP like Dr Dick is doing well, it doesn’t matter that Dr Snezana or Dr Iolanthe or Dr Jane is cross-subsidising the practice by doing the lower paid work.
It doesn’t matter that the commonest phrase they hear is “if I need something simple, I’ll go to Dr Dick, but when it’s really complicated, I come to you”.
It doesn’t matter that the receptionists pat a distressed mum on the shoulder and let her know she’s been booked in with “the lady doctor” because “Dr Dick is busy, but I’ll squeeze you in with Snezana/Io/Jane who is really lovely”.
It just happens that most (not all) the GPs who sweep up the difficult medicine and biopsychosocial complexity are women.
Given assistant health minister Ged Kearney’s deep commitment to eradicating medical misogyny it is unfortunate that the modelling of her government assumes the average GP is, well, male.
Before anyone tells me I’m sexist, women GPs on average, take 4-5 minutes longer per consultation. This is critical to their financial wellbeing.
It is somewhat ironic that a government that has rested heavily on a narrative of sexist patriarchal medicine ignoring/gaslighting/scapegoating women patients is doing exactly the same thing to doctors.
It doesn’t need to be this way.
Related
Dr Dick is probably a good, empathic doctor who would be happy to see Dr Jane’s patients. I’m sure Dr Jane would love to see some of Dr Dick’s patients. But, patients being patients, they choose their doctor. As one female GP put it “women cry to women but men also cry to women”.
The community, on average, assumes that Dr Jane is more empathic, more compassionate and (this is important) is more likely to see her practice as a calling or a vocation so they are more likely to bulk bill. She could also be working in a practice where she is exploited – particularly if she is an international medical graduate – and the more lucrative work is funnelled towards the men.
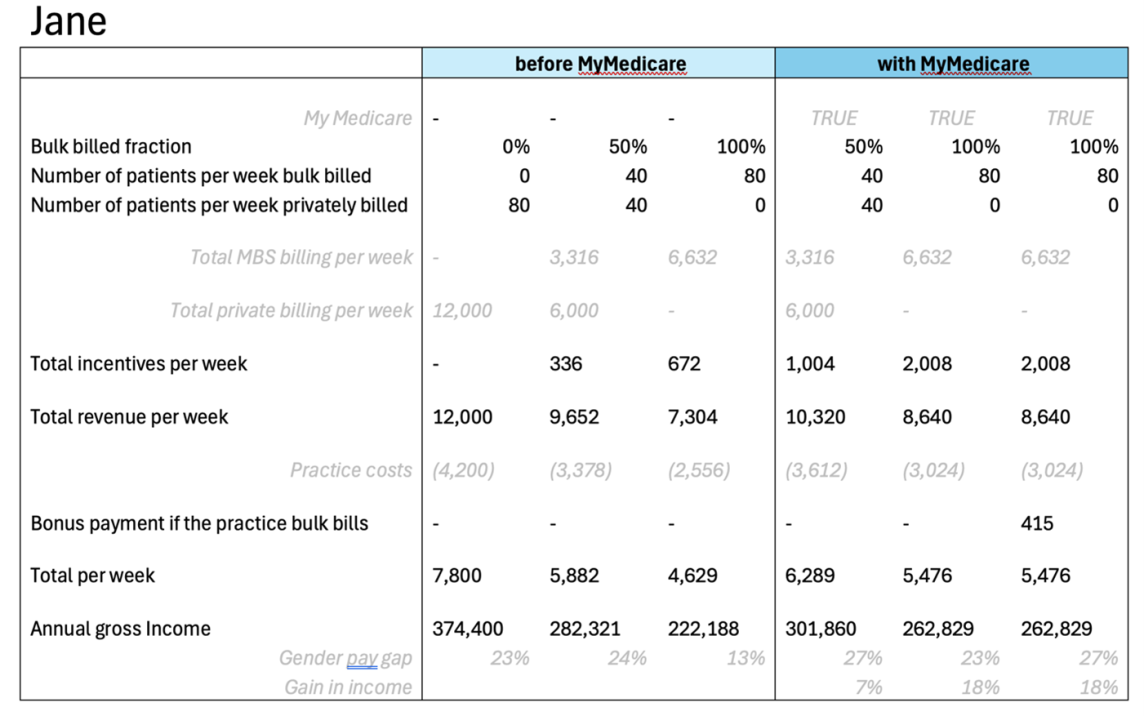
So let’s use the model for Dr Jane and keep the bulk-billing rates the same. She’s probably working less hours, because the emotional labour at home and at work is unsustainable for a fulltime load.
She is also probably cross-subsidising her income, because it’s harder to make ends meet. She is less financially stable because there is no maternity leave for contractors, she does the majority of the caring work, and has a lot less superannuation.
So, she is more financially stressed. Jane’s probably working at the UCC or in skin cancer medicine, or if she’s really smart, she’s marketing a skill she’s always had and setting up a menopause clinic doing what she always did but charging a lot more for the marketing of a “specialised practice”.
However, for the sake of argument, I’ve assumed Dr Jane is working 40 hours a week with two patients an hour and consistently charging an item 36. I’ve also assumed a 36 is around $150 for a private consultation, with 53% being concessional patients who are bulk billed 90% of the time. I’ll exclude her after-hours paperwork, which is probably around 10 hours a week.
Here’s what Dr Jane earns.
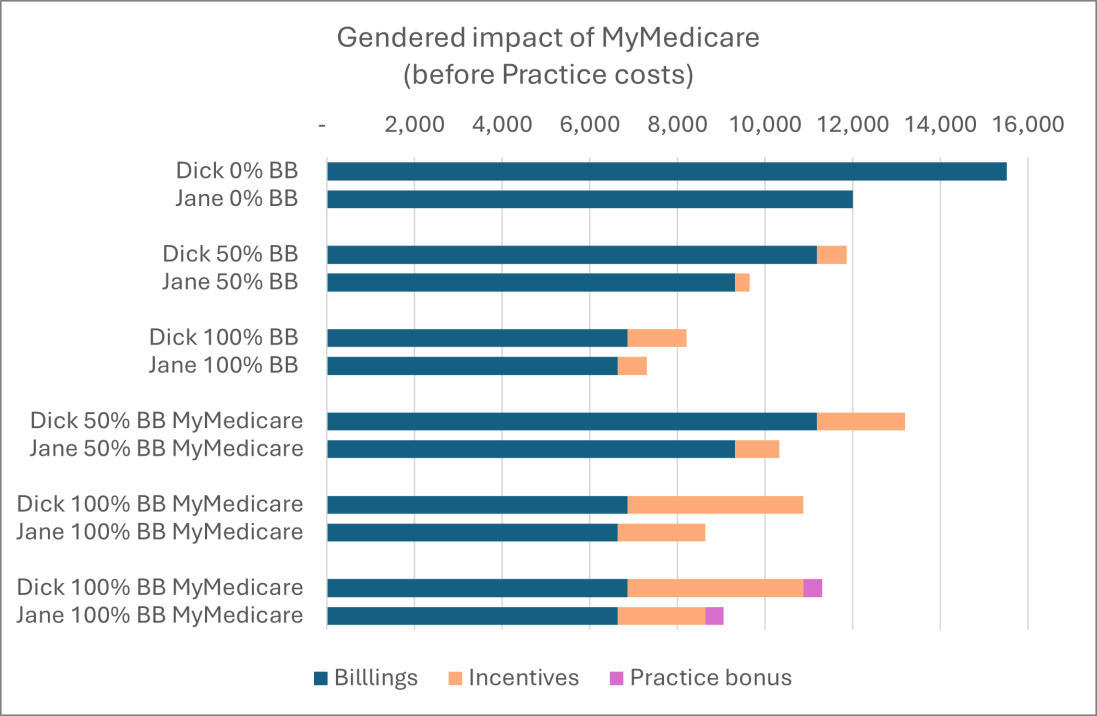
And here’s the combined graph, just to drive it home.
Oh, and the gender pay gap difference, which is worse.
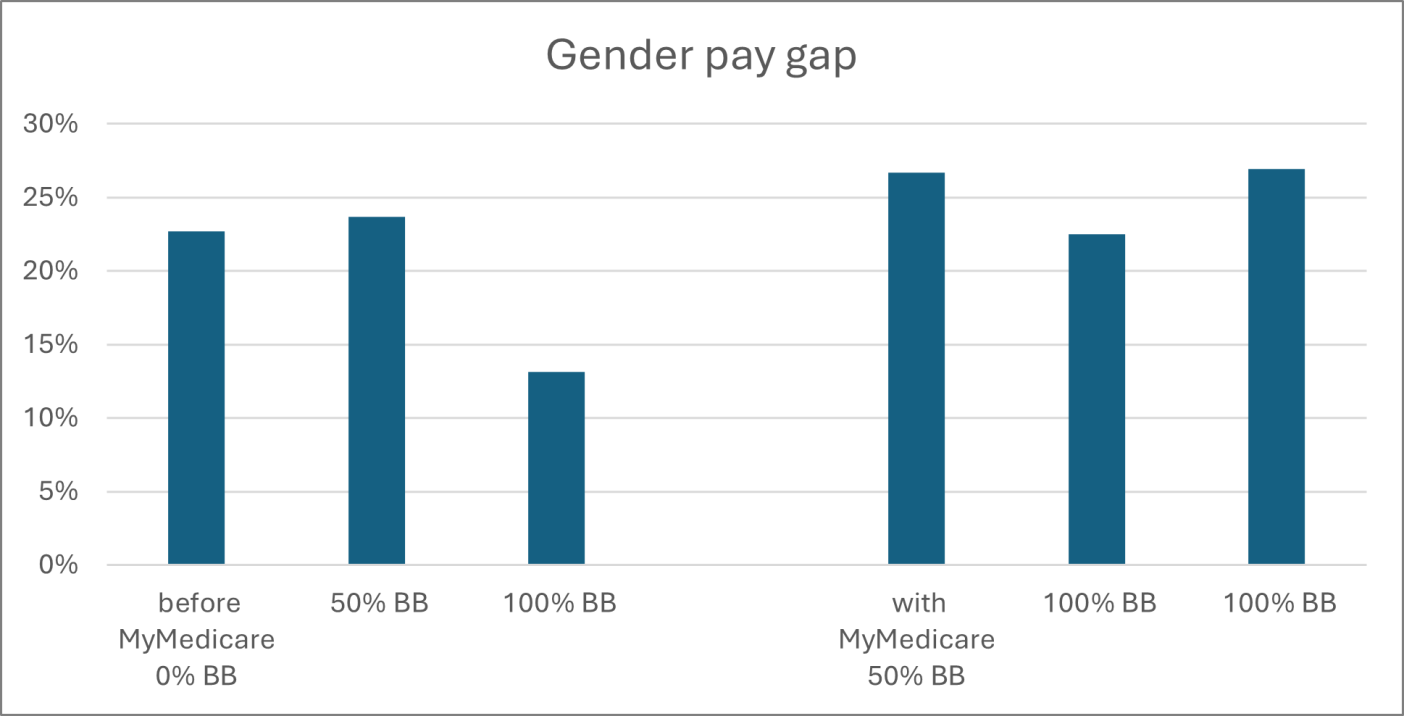
It is ironic that a government that is so strongly against “medical misogyny” has designed a policy that exploits women and the work they tend to do.
Every time I publish something like this, there will be comments that “many men do similar work”. Yes, they do. As I often say, the best GPs I’ve ever met involve the supervisors in my training team, who were unbelievably skilled and deeply empathic.
However, if it consistently “just happens” that women are disadvantaged by a policy, there is a problem. Here, the problem is that complex work is worth a lot less per minute than simple work. Which makes absolutely no sense. Particularly if you figure in an urgent care clinic, where managing a skin infection can drag in $10 a minute where an hour with a homeless adolescent with psychosis is probably around $2.
And the more straightforward work inside an item 23 is highly likely to be appropriate for the pharmacist, the nurse practitioner, the nurse-led clinic, the urgent care clinic and many other more highly subsidised services. Mainly because it is more likely to be a transaction with a consumer, eg “I need a script/review of my medications/treatment of my infection/dressing of my wound/preventive care”.
For Jane, most of her patients have nowhere else to go. None of the other services have longitudinal options for highly complex multimorbid care with a large dose of trauma and mental illness thrown in for good measure.
When everyone and their dog tells me they are “freeing me up” to do more complex work, they are actually “freeing me up” to earn a lot less for doing a lot more with no support in an environment where everyone and their dog talks about GPs like they are intellectually challenged.
Ministers, My Medicare is channelling all its energies toward the middle of the population – the Goldilocks zone of not too sick but sick enough.
I and my colleagues are tired of being the domestic servants of primary care, sweeping up after the parade of more “specialised” services have picked off the lucrative and arguably simpler bits.
The government has access to far more skilled economists than me. Policies do what they are designed to do, so I think we need a bit of a rethink.
My Medicare will make male GPs richer, and women GPs poorer. It will privilege the patients who are already doing well, and dis-privilege the complex patients hanging onto life by their fingernails. Here’s a simple way to understand the problem.
If the women GPs looking after complex patients want to continue working, they are going to have to privately bill the most vulnerable to provide decent care, enduring the community backlash for their “greed”. It’s probably why a third of the female GP workforce are planning to leave. The moral injury is too deep.
In my view, this move is an excellent example of policy misogyny. Ironically, when Ms Kearney talks about the harms associated with defining the average patient as a white male, her government is doing the same with their modelling for GPs.
It’s not right, it’s not fair and it’s not honest.
Associate Professor Louise Stone is a working GP who researches the social foundations of medicine in the ANU Medical School. She tweets @GPswampwarrior.





