The government has a lot of work to do convincing GPs that voluntary patient enrolment is a good thing for them.
Voluntary patient enrolment, now to be known as MyMedicare, took another step towards reality in this week’s federal budget. But GPs are sceptical.
Backed by the RACGP and AMA, and touted as a blended funding model that better reflects the chronic care GPs need to be giving, the proposal conjures for many the spectre of NHS-style capitation.
The details, where the devil famously resides, are yet to come. The budget does not say how much an enrolled patient is worth to the practice or the GP – nor whether payments will be made to the practice or to the GP, which could be relevant for payroll tax liability.
Last year then-RACGP president Adjunct Professor Karen Price told TMR fears of VPE were based on a misunderstanding of the proposed Australian model.
“Multi-source funding is not capitation, and the college is not in favour of capitation, of having the medical profession coerced or managed by health bureaucrats who really don’t understand each individual consultation,” Professor Price said. “We can’t have unelected people deciding what happens in a consultation room. That would be a destruction of the profession.”
But according to Australian Society for General Practice founder Dr Chris Irwin, VPE will ultimately lead to a further erosion of rebates and more government control of general practice.
Speaking to TMR this week after launching a petition for the peak doctor bodies to survey GPs about VPE, Dr Irwin promised to “just shut up” if a majority of GPs were in favour.
“I am absolutely sure that would not be the outcome,” he said.
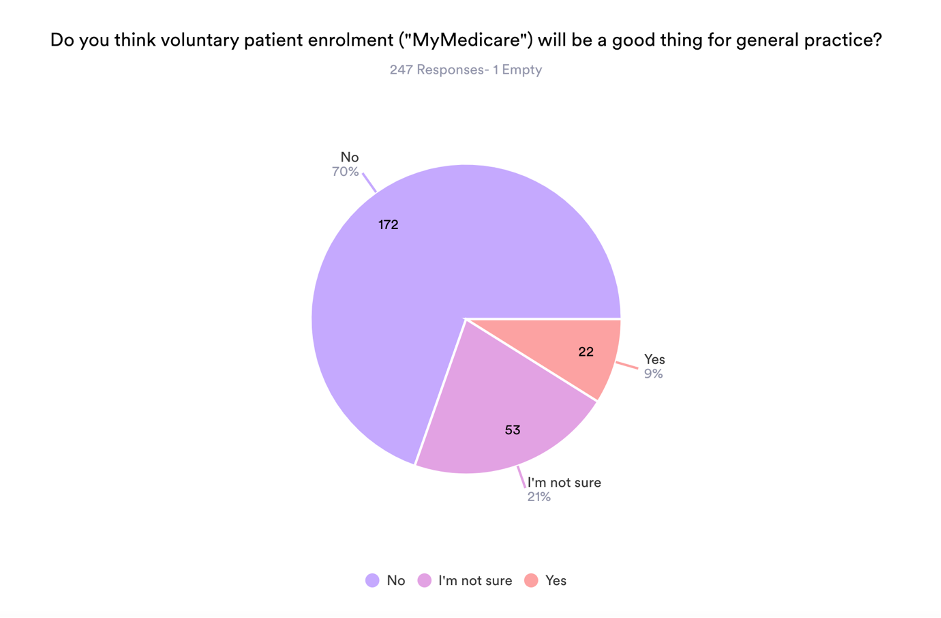
A small, back-of-the-envelope survey by TMR confirms his instincts.
Asked “Do you think voluntary patient enrolment (‘MyMedicare’) will be a good thing for general practice?”, 70% of the nearly 250 respondents (who were 97% GPs) said no.
Nine percent said yes, and 21% were unsure.
More than 140 respondents left a comment as to why they did or did not think VPE would be good for general practice. Here’s a sample of your comments, edited for readability and grouped according to the respondent’s answer to the first question.
Yes
- Supports GP-patient relationship, builds trust, rewards continuing comprehensive care and quality parameters, builds practice team capacity, aids identification and management of practice population. Success will obviously depend on govt’s approach and willingness to invest in value and outcomes over time.
- Fee for service is in conflict with the model of care. Fee for service has had its day. It’s time for blended funding to support team-based care.
- On condition that GPs who look after people with chronic diseases and coordinate their care will be remunerated more than GPs who do 10-min consults.
- It will allow GPs and practices to better define and understand our patient populations and therefore deliver appropriate health services individually and as a collective. Pooled funding will allow multidisciplinary care allowing me to get back to the parts of the job which really need a GP – diagnostic skill, patient relationships and illness management, with support from a team including social workers, dietitians etc. It will put the onus on government and digital health services to support me with the necessary digital health information and tools to look after my defined patient population. It still allows the flexibility to charge privately and to choose how I look after my patients. I will finally be paid for the clinical leadership and non-face-to-face care I provide.
- It will encourage continuity. Proactive care will be easier because practices will understand their populations. Equity funding can be provided to practices delivering desired outcomes.
Not sure
- I need more information, and detail. I’m concerned that it will mean more work for less money. If VPE stops random practices from doing care plans etc, fine, but if there is less fee for service and more indirect funding, contractor GPs will suffer … and leave.
- UK general practice has been complaining about VPE-style practice for years – we just need to be paid more to spend more quality time with patients to enable us to address the burgeoning wave of weight gain related illnesses and depression / anxiety issues in the community. The current system rewards quick appointments in high numbers.
- How can we make any decisons on this when we have absolutely no detail on what this involves or how it will be funded etc.?
- We need to known the $ amount & conditions attached to the funding. If it is not too restrictive on practices it might be the much needed funding boost that general practice is screaming for, but, it could all too easily become another political spin giving with one hand whilst taking with the other. General practice has nothing more to give back. We are at our financial & emotional wits’ end […] We as GPs & practices, are no longer able to subsidise general practice. I still remember the medical home model to be first introduced by PHNs. It fell flat on its face during the trials as it was underfunded & not worth practices’ nor GPs’ time & effort.
- It will be irrelevant in our town. We’ve lost a few GPs to the city in the past 12 months, the neighbouring practices have too, so the patients who are now doctor-less want to come to our clinic, but we have enough work of our own. So what point is enrolment, if there isnt a GP or clinic to enrol with as they’re not taking new patients as they’re short of doctors???
- If the benefits include the following, then it should be a great improvement on current situation:
1. Link the registered patient and doctor/clinic to all hospitals and other providers so communications flow seamlessly
2. Only the practice/GP the patient is enrolled with can provide patient access to Medicare rebates for services such as health assessments, care plans, medication reviews, case conferencing, nurse items and other areas of chronic disease care
3. Full access of the patient to all MBS items for rebate against GP services and not restrict like the healthcare homes model
4. Reduce access of the patient to all MBS items for rebate against GP consultations provided by practices that the patient is not enrolled with
5. Quality improvement data relating to the care of enrolled patients should be compared with QI pip data of non enrolled patients at a practice
6. The annual enrolment payment should be at least $500 per patient. Also a population based approach to the enrollment payment should be included to reflect patients disadvantage and improve equity for practices in low SE areas to provide care and improve the incentive for GPs to work in areas of disadvantage.
7. No compulsion to bulk bill enrolled patients
No
- GPs will lose control, there will be all sorts of conditions in the longer term with endless obligations to satisfy each and every demand from patients and government officials. Poor remuneration will follow an initial enticement/honeymoon period to get GPs signed up. The introduction of the NHS in the UK lead to the greatest ever migration of medical practitioners out of the UK to other counties that supported private practice.
- Truly the start of capitation in disguise.
- Chronic care, while important, is not as important as the daily care of patient’s acute needs. That is why patients ring up to see a doctor on a day-to-day basis not to see if their HbA1C is improving. The skill of general practice is not in chronic care, it’s in diagnosis with minimal reliance on investigation.
- It is the beginning of capitation as in the UK. And that system is dreadful.
- Thin edge of the wedge to UK-style mess – the very reason I left the UK.
- It’s simply a method to limit government spending in primary care, and to control medicos more tightly.
- VPE will kill GP, the backbone of the healthcare system. It will further entrench a two-tier healthcare system as doctors exit the government-funded model to provide expert expediting care for those who are willing and able to pay while those who can’t pay will wait, and have worse outcomes, and the doctors serving them will burn out and leave in droves if they don’t commit suicide first.
- It will lead to even less funding for general practice.
- I do believe it will lead to more government control over general practice and eventually a full capitation style of funding model which we have seen has failed in the UK.
- Obscure funding models, KPIs, reduced rebates for fee for service. All leads to NHS-style care delivery model and we know what a balls up that is.
- Doesn’t solve any problems of primary care.
- Useless and unproven. Removes choice both for GP and patient.
- Because it will be used as a cost reduction tool and compromise the incomes of tenant GPs especially, yielding a further shortage of doctors who want to work in the GP area. It is a terrible idea and the RACGP and AMA should hang their heads in shame for not asking members what they actually want.
- The federal government, AMA and the RACGP must think we are all f@#king idiots. The only thing VPE will be good at, is losing an entire generation of GPs. Clowns.





