We are not a permanently open chatline and patients are not owed an answer about every non-urgent niggle.
In the past two weeks, three patients and I have mutually agreed to part ways as I have been unwilling to meet their non-urgent needs between appointments.
I’ve alluded to this before, but last week I hit a wall.
It came to me on reflection that I’ve inadvertently been encouraging this behaviour by getting staff to reply every time there is a detailed email (about a non-urgent medical concern) from a patient, often weeks after their appointment, with a quick “do this or make an appointment”.
Sometimes I’d go so far as to email them myself with a somewhat detailed reply, or give them a “quick” call up to 10 minutes, gratis, to ensure I was not missing anything urgent.
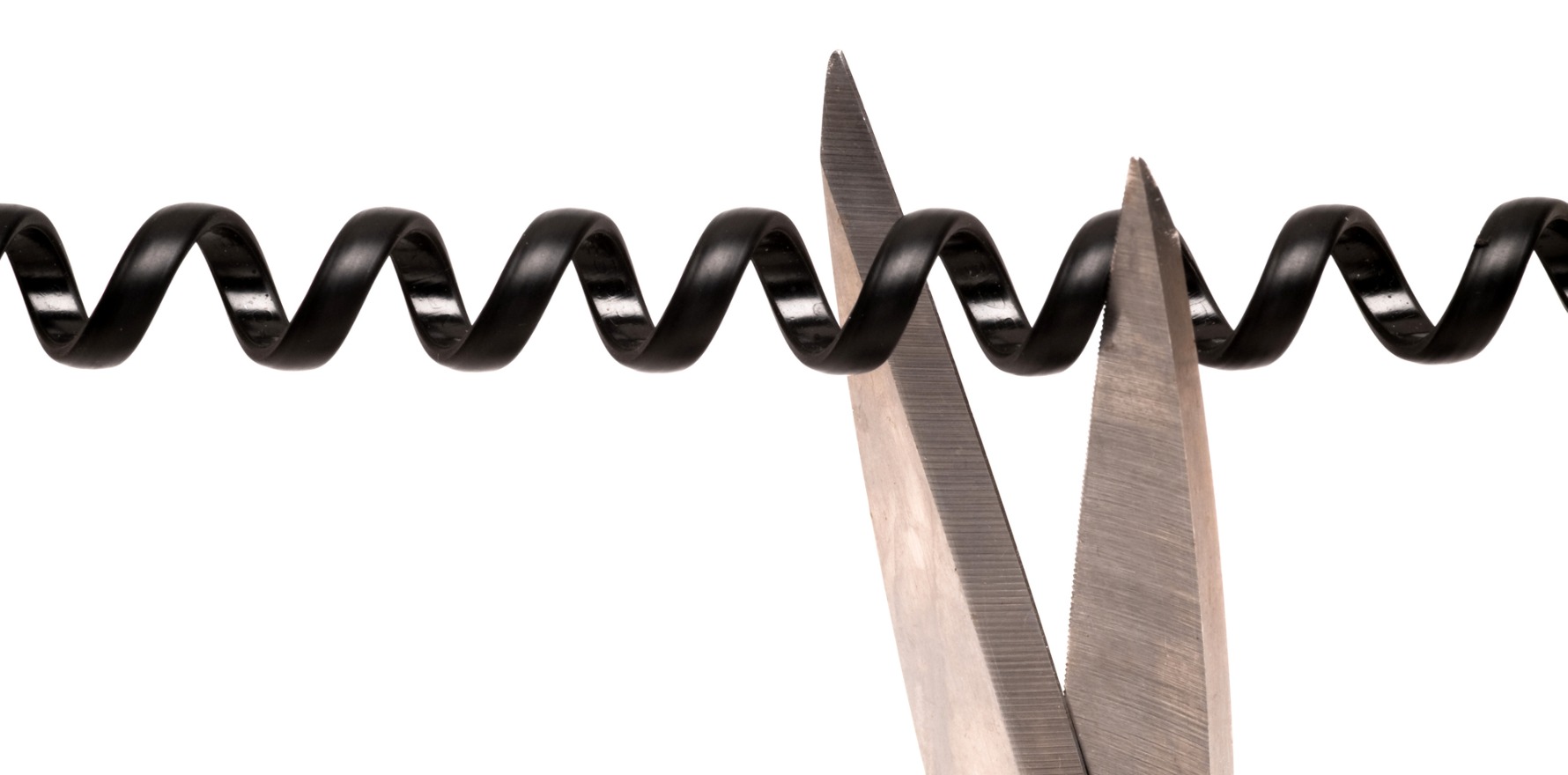
It’s December, we are all tired and as fellow GP Todd Cameron noted recently in a video on X, general practice tends to have a big head (what we do in clinic with the patient) followed by a long tail (what we do unpaid between visits and appointments that patients don’t see and therefore don’t appreciate) that over time adds up to many, many unpaid hours, disruption out of rostered hours and eventually, resentment and burnout.
For me, it came to a head because I complained about this to a male GP colleague and friend, whose reply was along the lines of “well, your staff can simply reply something like ‘in the interest of a prompt reply, I’m writing on behalf of Dr Joshi … ‘”
Except, as this colleague found out, I do not want to be emailed about non-urgent things that can wait till the next appointment. Once I know, I feel obliged to do something with the information. It is an open tab in the browser of my brain and adds to my mental load till I can close that loop.
I don’t want “Just so you know” or “I’m making a note of this to discuss at our next appointment” emails.
I don’t want “Could you please tell me the last two doses of my medication as I can’t recall and was just wondering how it compares to my current dose?” emails.
I don’t want “Could you ask her to call me, I have a spot on my face that is worrying me?” phone calls.
I don’t want “Could you get the doctor to fill this form out ASAP and send it back to me?” or “I’m overseas and haven’t seen you in eight weeks but [problem] – what should I do?”
These have all happened to most of us many times, I am sure.
Possibly to those of us who are female far more than male, because we also carry the burden of the “nice” tax.
Because I also have a social media presence, in the absence of timely responses to these emails I occasionally get DMs on my social media pages (and no, I should not have to not use an anonymous handle to avoid these) saying “I’ve emailed you and am awaiting a reply.”
So yes. I hit a wall.
I said to my colleague, “Wrong answer because they should NOT be emailing me about non-urgent stuff between appointments, full stop. And if they are worried about something enough, they need to request an appointment and be willing to pay for it.”
And because I was so incensed about it, I posted on a GPs-only page on Facebook to ask if I was out of touch and did most of my colleagues entertain this? The vast majority of my peers said “hell no”. About two (both men) suggested I could monetise it/use it as a means to engender patient loyalty.
In clinic, I raised this issue with the people who were the most recent offenders.
“Why was this so urgent it needed an email and (my) action prior to your booked appointment?” Silence.
“As we’ve seen with this paperwork and the questions I needed to ask you, it is very hard to fill these out in your absence, which is why I refused to do so asynchronously.” Silence.
“It is not possible to provide medical advice when I’ve not seen you in months and you’re not currently in Australia. It is safest if you see someone locally and make an appointment on your return.” Silence.
With each of these I stated that if caring for their safety and mine by refusing to engage in non-urgent asynchronous communication was upsetting or offensive to them, then I am not the doctor for them and they should look elsewhere.
Going forward, as we have clinical software that sends out reminder emails five days before an appointment and an SMS two days prior, we have clear autoreply that also states “Doctors do not check this email account nor do we provide medical advice via email. Please call to make an appointment.”
Staff likewise now know that if we get emailed non-urgent medical questions they are to offer patients an appointment.
Some of my patients are lawyers, who tell me emails, texts and DMs can be a way to “put you on receipt”, I.e. “I’ve notified you of my concern, the ball is now in your court.” Admittedly they do not work in medical law, but I’ve taken their word to heart. I do not wish to monetise this service by being on call for non-urgent queries and I do not wish to work even more unpaid hours doing administrative work because people forgot or were disorganised.
It can feel scary to set and to enforce boundaries, but for the most part, they have saved me more trouble longer term than not doing so.
Last week I was upset enough that I once again considered giving up my work and doing all the ED locums again, where I showed up to a shift, worked my butt off and then had ZERO responsibility and contactability outside of those hours.
It was bliss.
The other way, obviously, is to set and enforce boundaries that work. My patients know I will absolutely call them if there is something to discuss, or if there is a problem or I am worried about them. This gives my regulars the confidence to also know over time that they won’t have access to me outside of those circumstances and in clinic.
Ultimately, when many/most of us don’t do this, or invalidate those of us who do or give in because it’s easier, we set up unreasonable expectations for all of us, adding to our work challenges.
So as the end of the year looms, here’s to better boundaries in 2024, to patients who get it and support us in this, and continuing to love what we do without having to be a martyr to it.
Dr Imaan Joshi is a Sydney GP; she tweets @imaanjoshi.