Believe it or not, new legislation may make the process feel like a fairer fight.
Change is afoot at the Professional Services Review, with a three-fold increase in “no further action” findings and new legislation dictating the makeup of review committees.
The PSR, which investigates cases of potential inappropriate practices relating to Medicare, elected to take no further action in 19 cases during the last financial year, compared to just six in the previous year.
There was also a slight drop in the total number of cases referred by the Chief Executive of Medicare, from 108 in 2021-22 to 91 in 2022-23.
A finding of no further action is essentially the PSR director deciding, after an investigation considering all the relevant material, not to force the clinician to repay any Medicare benefits.
For all intents and purposes it’s a not-guilty verdict.
In instances where the PSR does take further action, some practitioners are asked to negotiate an agreement where they acknowledge wrongdoing and potentially repay some Medicare benefits.
The rest of the doctors are referred to a committee of peers for further investigation.
Doctors who reach the committee stage rarely come out unscathed; a committee has only handed down one case in the last three or so years with a finding of no inappropriate practice.
A rise in the number of no-further-investigation findings, then, is good news.
Putting the numbers into context, in the 2021 financial year the PSR only decided to take no further action around once every 20 cases, but in 2022 it decided to take no further action once in every five cases.
It’s a dramatic return to form for the agency, which has been operating under Acting Director Dr Antonio Di Dio, a Canberra GP, since former director Professor Julie Quinlivan’s departure in May 2022.
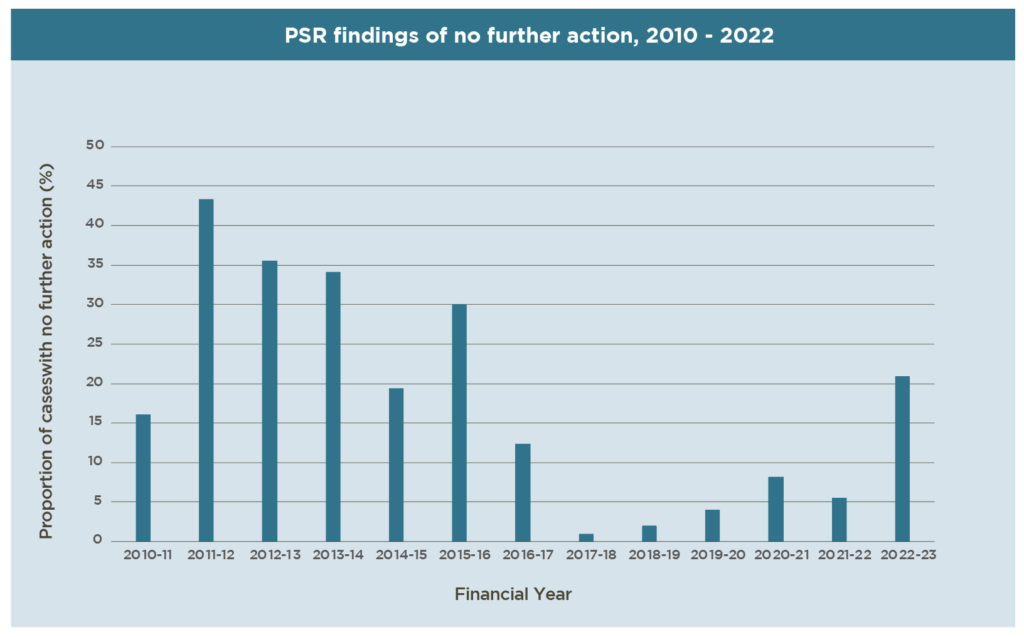
Looking back at PSR’s annual reports since 2010, it was previously typical for the agency to take no further action between 10% and 35% of the time.
In the 2015 financial year, for example, it took no further action in 30% of cases.
While this wasn’t even a high-water mark for the agency – in 2011, it reached 43% with no further action – the no-further-action findings dropped off a cliff in following years: in 2016-17, it dropped to 12% and in 2017-18 it dropped to less than 1%.
Professor Quinlivan started her three-year term as director in February 2017, just as the no-further-actions findings started to fall.
The highest proportion of no-further-action findings under Professor Quinlivan was 8%, in 2020.
The PSR’s 2023 annual report also offers insight into the way the agency operates.
GPs are still overrepresented among the cases that proceed to a committee stage; of the 16 committee cases in 2022, 11 of the people under review were GPs.
Telehealth was a particular compliance focus this year.
In the cases where the director elected to take no further action, he cited high-quality notes and appropriate billing for the situation as important factors.
“In general, telehealth services related to brief and standard consultations and were largely deemed appropriate by peers,” the report reads.
“However, telehealth services conducted by phone for longer consultations (particularly general practitioner Level C and D attendances) and services such as chronic disease management, health assessments and mental health services were more likely to be found to be inappropriate.”
The report also noted a “concerning trend” of doctors appearing to copy and paste clinical notes across patients.
The most common GP Medicare items that came under review were 3, 23, 36 and 44, or level A, B, C and D consults.
GP mental health items 2713 (along with telephone equivalent 92115) and 2715, along with Indigenous health item 715 were also among the most investigated.
The video telehealth equivalents of these items were not typically of concern.
Items 92115, 2715 and 715 are newcomers, in that they did not appear on the top-10 list of audited item numbers released by the PSR earlier this year.
Poor records and a lack of evidence of clinical input were the chief concerns cited by the PSR in these cases.
“There is a need for practitioners to balance their workload to ensure there is sufficient time to make accurate clinical notes in patient records … the reliance on electronic autofill in some entries may also aggravate the risk of poor notes that do not reflect the content of a consultation,” it said.
Skin medicine also continued to be of particular concern.
Alongside the typical concerns over inadequate documentation and poor clinical input, the PSR said it was concerned about a lack of consent for invasive procedures and clinically unnecessary skin flap repairs.
“Typical examples include situations where a flap was performed in an area with sufficient skin properties or a small lesion size, which the general body of peers may consider that an elliptical closure would have been sufficient,” the PSR said.
For GPs with a special interest in dermatology who find themselves facing a committee, new legislation might prove key.
Under previous rules, the committee of peers had to be made up of consultant physicians of the same specialty that the doctor under investigation was acting in at the time of the incident.
New rules laid out in the Health Insurance Amendment (Professional Services Review Scheme No. 2) Bill 2023, which has been passed, clarify that if the practitioner rendered services as more than one kind of specialist – e.g. a GP with special interest in dermatology – then the review panel must include peers from both specialties.
In the past, a GP dermatologist might have faced a panel of only dermatologists or only GPs; now, the panel would have an even mix of GPs, dermatologists and/or GPs with a special interest in dermatology.
It’s a subtle change, but one that may prove meaningful to doctors facing a committee.
Other changes under the bill include a requirement for doctors who are unable to attend a hearing for a medical reason to supply a medical certificate, as well as an allowance for the PSR director to extend the statutory timeframe for deciding a matter if the person under review leaves the country or has ongoing court proceedings.