Bupa wants to develop care provision alongside insurance to the point where up to 30% of its members’ healthcare encounters never leave the Bupa ecosystem. The government should probably wonder what might happen if it succeeds.
We are all witness to the big emerging trend of private health insurers moving to provide healthcare instead of just funding it.
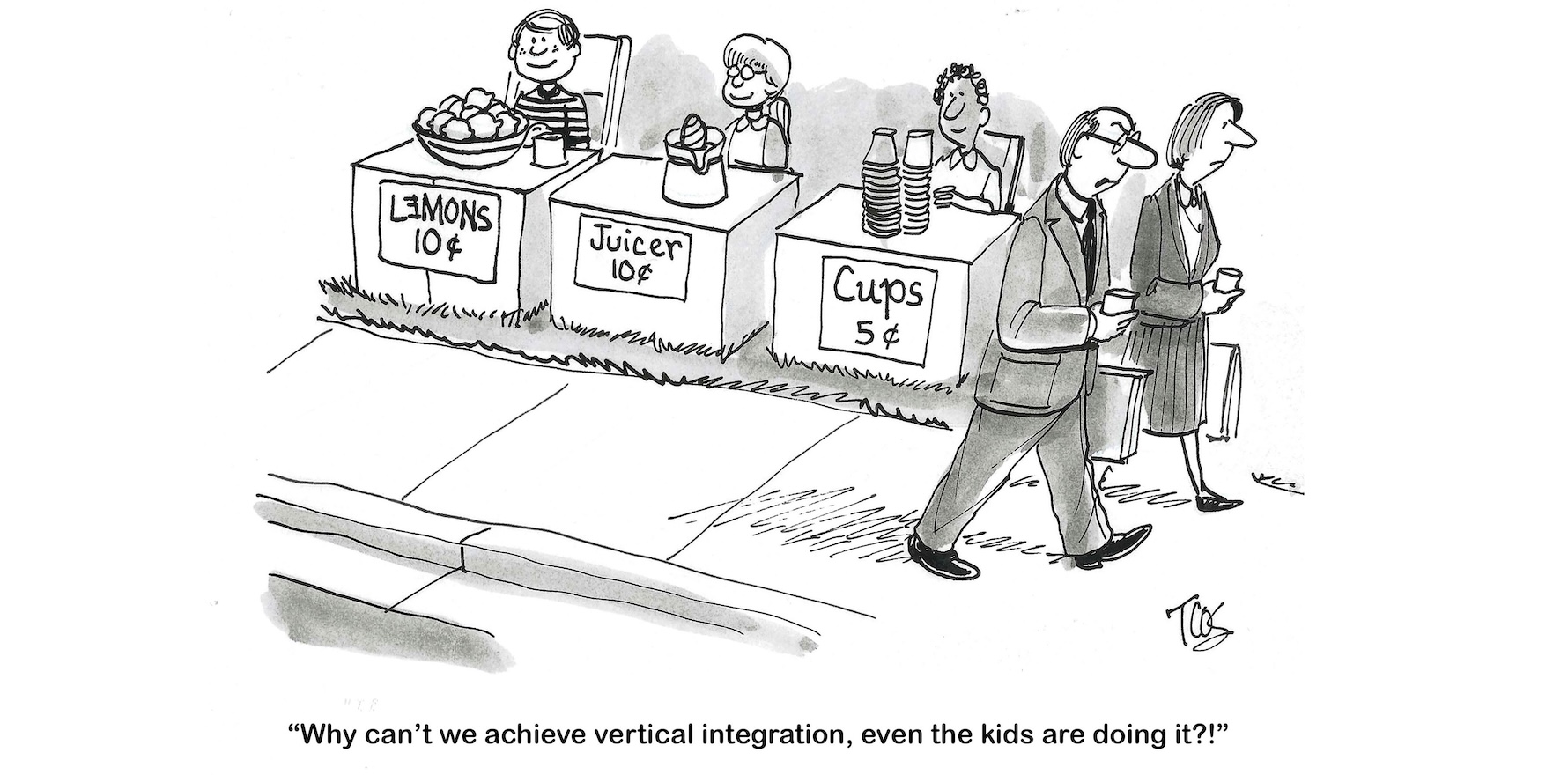
Doctors think that the PHIs are trying to vertically integrate in the manner of the US insurers – whose model involves controlling the entire patient care chain to optimise costs, often by directing care and thereby bypassing clinician autonomy – but the insurers have so far argued that they have to participate in care because the current funding system promotes and maintains inefficient and out-of-date models of care.
They want to disrupt the system by introducing more efficient and innovative models of care, such as cloud-based virtual care models, and the only way they think they can do that is by getting into the provision game and fixing it from within.
Who does the government and public believe?
A big hint as to what might be going on may have been dropped this week by the global CEO of BUPA, Inaki Ereno, who was in Australia and did an exclusive interview with the Australian Financial Review, in which he said:
“Bupa should aspire to have 25% or 30% of the cases, the claims, of the episodes that we manage going through an ecosystem that we own. We need to own 25% to 30% of those cases. We need to know the cost of things.”
You can read more about that in our story, here.
How does one read such an aspiration?
In one respect it sounds entirely like a plan to vertically integrate for cost control, just like the doctors are starting to worry about.
Mr Enero seems to clearly be saying he wants 30% of all provider services — transactions and the costs – running entirely within his group’s ability to run and control the costs.
This isn’t strictly US-style insurance. Their model is run 100% through your ecosystem and own it all, from hospitals to general practice and allied health in a line so you have supply chain management in a good tight line.
But it isn’t what successive Australian governments since 1971 have envisaged the role of PHIs to be – and why we have had subsidised the sector, at times up to $9 billion per annum – in complementing the public system to help with hospital and specialist costs.
It’s going way beyond that now.
Is there a chance 30% might end up like being a “little bit pregnant”? If 30% works well, why not 40%, and so on?
A lot of private health insurance initiatives on innovative new care models are really interesting and potentially would not be funded and developed as thoroughly without the private sector push.
A big problem here, and one reason why the PHIs are pushing the limits on regulation and policy with this push into vertical integration, is that the sector is right when it says that the system is funding and rewarding outdated and inefficient models of care.
Virtual care, hospital-in-the-home technologies and services, telehealth, new cloud-based care platforms are all being retarded significantly by the fact that the healthcare system funding paradigm, and to some extent national policy on new care models, is significantly holding back the massive potential of these new models of care in the system.
Through this, PHIs are wearing costs they feel that should not be wearing.
Related
For years the government has prevaricated on what the role of the private health insurers actually is in the system and just how it should or should not support them.
Now the private health insurers, who prior to covid were in a death spiral that no one thought they would pull out of, aren’t waiting around to see if the system eventually equalises to what they were facing prior to covid.
Whether you love them or hate them you can’t blame them for starting to push the envelope while they can – they are now more profitable and powerful than at any time in their history – to ensure that they have a long-term future in the system.
Which means the government needs to give a lot more immediate term thought to what the PHIs’ role actually is in the system and how they can be sustainable long term as a complement to the system from which the public gets a good return on investment (unlike in the US).
This thinking might have to include new guardrails and regulation beyond things like the Health Insurance Act preventing the PHIs from subsidising any form of primary care that is funded already by Medicare. Ideally it would address the frustration that the PHIs have around the funding of much more modern and efficient care models as well.
The PHIs’ march into general practice and telehealth at scale possibly provides a good early example of the sort of things that could eventually go wrong if we don’t get some more clarity soon.
In this week’s announcement that they’d like to essentially vertically integrate at least 30% of the health system encounters of its members within its own ecosystem, Bupa also announced its intention to own up to 130 GP medical centres within three years.
That would likely make Bupa the second largest GP corporate in the country, treating something like 1.6 million patients via 8 million consultations through 1400 GPs per year.
Bupa has about 4.5 million customers in Australia. Is it then just a coincidence that 1.6 million potential new Bupa GP patients equals about 30% of their customer base, which would go to the idea that Bupa wants 30% of all their customer healthcare interactions held within their own ecosystem?
Seems a bit far-fetched, even to me. But let’s go with it.
If that’s what Bupa is trying to do, it is clearly going to try to influence in some way or provide some form of incentive from other parts of its ecosystem for 30% of its members to go and see Bupa GPs.
And surely Bupa isn’t just going to run one of Australia’s largest GP practice networks and not leverage that patient influence to push its members back through other parts of its ecosystem – that’s sort of what Ereno is alluding to above. It’s what Sonic do and, back in its day, Primary Healthcare did to channel more tests to their upstream pathology businesses.
And what is Bupa going to do with all that patient data it is generating through its shiny new giant GP network?
It would likely be very useful in optimising the costs of that patient’s management across its ecosystem if it can work out a way to use it. Notably Bupa is very keen on sequencing the DNA of as many of its members as it can to “optimise” their care over time so it’s not like it isn’t getting into data big time.
Is this now against the law (the Health Insurance Act) and is it crossing other informal or even formal (privacy and consent) system boundaries that the federal government so far hasn’t properly contemplated?
Bupa, like any good business, is just pushing the envelope of what is possible, possibly wondering when the government might actually arc up.
But while the role of PHIs remains as blurry as it has been over the years this could easily end up in bad places for patients and the system. It might even end up bad for the PHIs themselves if they invest a lot of money in something the government ultimately finds it needs to regulate much more tightly.
Witness how the government has let private telehealth platforms operate outside of Medicare because they effectively didn’t have any governance or regulation in place. It wasn’t in front of how fast these entrepreneurs and technology could move if they did everything outside of Medicare.
Now we have a whole powerful new emerging ecosystem of private providers operating outside what a lot of doctors, and some government policymakers think are good rules to keep patients safe and the system efficient.
This week it was also revealed that Bupa may have a tilt at buying some or all of the distressed Healthscope private hospital network – that would fill a nice gap for its 30% plan – GPs, hospitals, dental, optical … it certainly seems to be aiming for a full set to run an enclosed vertically integrated ecosystem of private care where it can.
Again, not pointing the finger particularly at Bupa here for anything dastardly. It and the other big private PHIs are only doing what for-profit groups need to do – ensure they keep making a profit. And why wouldn’t they want to be pushing the boundaries after the near-death experience they all had prior to covid.
As painful and difficult as the process would be, the government needs to quickly become more proactive in defining what role the PHIs can play in the system moving forward and how, rather than letting the PHIs try to define most of it themselves.
Health Services Daily will deal with the topic of private providers in promoting more efficient innovative models of care to keep hospital costs in check at its upcoming New Care Models in Reshaping the Future of Hospitals Summit on 16 October at the UTS Aerial Centre in Sydney.
You can check out the program and speakers and get your early bird ticket here.