But the big question is what happens next?
Education and opportunistic testing are needed as STI notification levels return to pre-covid levels, according to two Aussie experts.
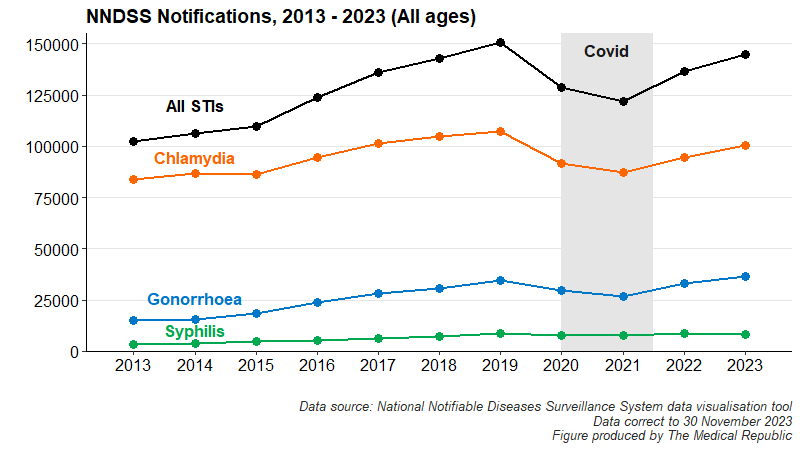
In November, newsGP reported Australia was experiencing a surge in common STIs: a 45% increase in gonorrhoea notifications and a 24% increase in chlamydia notifications from 2021 to 2023.
And while the data, taken from the National Notifiable Diseases Surveillance System, are technically correct, a closer look reveals we have returned to “normal” pre-covid trends, with the dip in notification frequency explained – in part – by heavily reduced testing during the pandemic.
Associate Professor Jason Ong, an academic sexual health physician from the Melbourne Sexual Health Centre, said it was unfair to only compare data from 2021 onwards.
“We have to be cautious about seeing this rapid surge. If we take a step back and look at 10 years [of data], rather than a two- or three-year time span, then we definitely see a little hiccup during covid [but overall] the lines continue to increase,” he said.
“This tells me we’re not testing enough [and] we’re not treating STIs enough. Despite that little blip in covid, we still have not really controlled any of these epidemics – chlamydia, gonorrhoea or syphilis.”
Dr Sara Whitburn, chair of the RACGP sexual health medicine special interest group, agreed with Professor Ong’s assessment but emphasised the importance of keeping an eye on what happens over the next 12-24 months.
“I hope [STI notifications] go up for a little bit, as that means we’re talking about sexual testing and sexual health more. Then as we start to improve testing, treating and sexual health education – both clinically and also in the broader community and schools – then I hope it would plateau,” she told The Medical Republic.
Researchers from the Kirby Institute are worried the increases in diagnoses seen in the last decade are likely to continue in the coming years.
Related
“Any rise in STIs is bad news, but rising STIs against a backdrop of decreased testing, and the persistent upward trend over the past decade, is particularly concerning,” said epidemiologist Dr Skye McGregor in a statement accompanying the release of the Institute’s latest annual report on STI trends in December last year.
But the post-pandemic return to “normal” is not the only reason why we are seeing an uptick in STI notifications. Condom use is declining among young people and people using PrEP to decrease their HIV risk.
“[Some people] will use PrEP on demand and then take doxycycline to decrease their transmission of syphilis as well. It’s fantastic that [there’s] good protection for these specific organisms – but don’t forget the condom. We’ve got these great things, but we want to make sure they’re all working together,” Dr Whitburn explained.
Dr Whitburn recommended incorporating asymptomatic and opportunistic STI testing into other related consults, such as asking about sexual health when undertaking a contraception consult or during screening for cervical cancer, noting self-collected vaginal swabs for STIs were also a possibility.
“People don’t always want to volunteer things around sexual health, but don’t mind being asked. When you’re seeing people at other times, [it’s worth] saying, ‘I just want to check in with you – have you had any concerns around your health? I asked about your heart health. I asked about your musculoskeletal health. Can I ask you about your sexual health as well?’,” she said.
Professor Ong echoed Dr Whitburn’s comments around taking advantage of opportunistic testing, noting GPs shouldn’t just rely on a cancer screening once every five years to discuss sexual health.
“If we are going to be testing less and less frequently, [then] that’s going to have a significant impact on STIs,” he said.






