The OECD PaRIS Health Survey provides the first robust international evidence capturing patients’ voices on their experiences in primary healthcare, and how this translates into health outcomes.
This morning, I saw an 85-year-old non-English speaking patient who I’ll call Zahra.
I see Zahra a lot as she has multiple chronic conditions, including a range of autoimmune diseases, fatigue, cognitive impairment and pain.
Over the years, she has often arrived with one of her five adult children, who in wanting the best for their mother pushed me to do something, even though we’d discussed many times that more intervention wouldn’t necessarily improve her health.
Zahra’s life became a merry-go-round of specialist appointments.
At one stage, I sent her to a pain clinic, which did not go smoothly. Zahra was administered opioids and became very confused; soon her kidney function deteriorated, and her blood pressure rose, leading to a hospital admission.
Since then, my conversations with the family have been focused on treatment goals. We’ve discussed the children’s and Zahra’s wishes and agreed that keeping her comfortable is our primary objective rather than searching for any underlying pathology. Her quality of life has improved.
As GPs managing the tide of chronic disease in Australia, we know intuitively that patients do better when their care is well coordinated, and when it reflects what they value most.
To meet their needs, we need to be person-centred and support individuals to have the best quality of life they can, while helping them navigate the health system. We can, of course, do this much better when we get to know the patient over time and there is continuity of care.
In Zahra’s case, factors such as social isolation, language and cultural differences mean she is more vulnerable in the healthcare system, so having a healthcare professional who can tailor care specifically to her needs is especially important.
Related
Probing what patients want
Despite a large amount of available health data, the fact is we know very little about what patients actually want, and whether the Australian primary healthcare system is meeting these needs.
That is, until now.
Australia recently participated in the first internationally validated survey capturing patients’ voices on how their chronic conditions are managed in primary healthcare, and how that translates into health outcomes.
The Patient-Reported Indicator Surveys (PaRIS) is an international survey run by the Organization for Economic Cooperation and Development (OECD) in 19 countries. In Australia, it was implemented by the Australian Commission on Safety and Quality in Health Care with ORIMA Research on behalf of the Australian government’s Department of Health, Disability and Ageing.
The survey was completed by 54 GP practices in Australia from 8 June to 20 December 2023. They recruited patients with chronic conditions aged 45 year and over who had attended the practice in the last six months; 2392 participants were included in the results.
PaRIS collected the first Australia-wide data on PROMs (patient-reported outcomes) and PREMs (patient-reported experience) measures.
Unlike patient satisfaction surveys, which largely provide data on patients’ experiences as consumers, PaRIS provides deep, rich insights into how patients feel the primary healthcare system is managing chronic conditions in Australia.
PaRIS data paints a positive picture
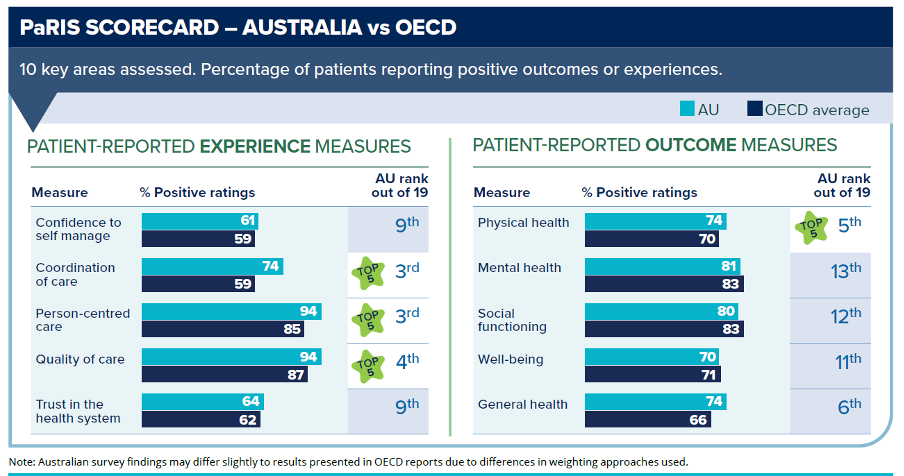
The results show that Australia is doing well by OECD standards. We are among the top few countries in the OECD for:
- Quality of care – 94% of Australian patients with chronic conditions reported positive experiences at their GP practice in the last 12 months, compared with the OECD average of 87%;
- Person-centred care – 94% of patients rated person-centred care positively, compared with the OECD average of 85%;
- Coordination of care – 74% of patients rated their care coordination positively, well above the OECD average of 59%. Care coordination improved with patients’ age and their number of chronic conditions, indicating we’re targeting our services to those with the greatest need.
The survey found that more positive patient experiences are linked to more positive health outcomes, with those who experience better quality healthcare more likely to report better physical health, mental health and wellbeing.
Patients who take an active role in their own care – those who have higher confidence to self-manage their care and who actively seek health information – have markedly better outcomes than those who do not.
The survey highlights the value of patients having a single GP to manage most of their conditions.
Quality of care was rated positively by 97% of patients who had seen a single GP for 3 to 5 years, compared to only 79% of patients who did not see the same GP. Similarly, 78% of patients who had seen a single GP for three to five years reported positive experiences with care coordination, compared with only 29% of those who did not see the same GP.
Interestingly, those patients who had a high level of trust in their health professional also had a higher level of trust in the entire health system. It’s an affirming finding for GPs and highlights the central importance of the patient-doctor relationship.
Tackling the digital and communication divide
The PaRIS Survey also unearthed some opportunities for improvement.
Around one-quarter of Australian patients indicated they had to repeat information that should have been in their health records in the past 12 months.
These patients were less likely to say they experienced person-centred care, rate their last consultation positively, trust their doctor at their last visit, or trust the health system overall.
Although most of us already try to be patient-centred in terms of care planning, the survey showed there was a disconnect between GPs reporting they had written a care plan and patients knowing of its existence.
This highlights again the importance of working with the patient, helping them identify their goals, and making sure that they understand the care plan when you give it to them.
There were also gaps in patient awareness of digital health services, which were commonly offered in Australia. For example, while 60% of providers offered video consultations, only 40% of patients were aware their practice offered this service.
The 13% of patients who reported difficulty in accessing information from their provider’s website recorded lower outcomes and experiences than those who found this easy, including for quality of care, trust in their GP and coordination of care.
Discussion of risk factors for chronic disease could also be better targeted. Patients with chronic conditions were more likely to be classified as higher risk based on their physical activity levels and alcohol consumption than for diet and use of tobacco – but discussions about alcohol use with their GP was less common.
Translating findings into better outcomes
This ground-breaking survey has some important implications for GPs.
First, taking part in the survey has been incredibly valuable for participating GP practices as it has provided a unique opportunity to examine their own patient cohort. The patient-reported data was linked directly back to practices, enabling them to make changes that are already improving patient experiences and outcomes.
Second, the findings support the value for GP practices of signing up to MyMedicare, which promotes continuity of care, provides new longer telehealth items, supports regular health assessments, and provides chronic condition management items.
And third, the survey confirms that Australia’s primary healthcare system is performing well compared to other countries. As our health system continues to evolve, we really need to hold onto the elements of that system that patients value.
What our patients want is someone who can listen to them, help them identify what are the important goals, simplify health information, manage their expectations, and reassure them around the things they don’t need to worry about.
If our patients have positive experiences, we’re going to get better feedback and gain more satisfaction from our work. Patient outcomes will improve, and we’ll feel like we’re actually doing a great job. And don’t we all want to feel like that?
Associate Professor Liz Marles is a clinical director for the Australian Commission on Safety and Quality in Health Care and a GP. She is currently chair of Therapeutic Guidelines, past president of the Royal Australian College of General Practitioners and a member of the RACGP Council.





