The long stride walking test can help identify ischiofemoral impingement in patients with posterior hip pain.
A 65-year-old woman presents with chronic left buttock pain for approximately 10 months, with a recent exacerbation after incidental minor trauma.
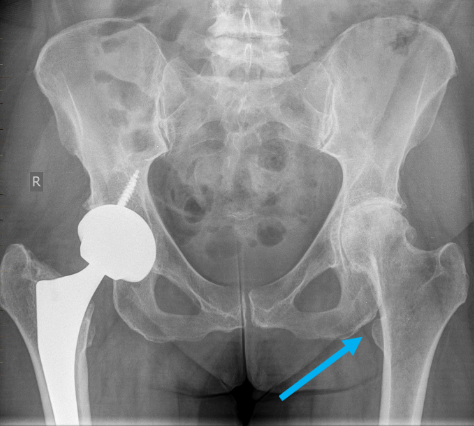
She has had longstanding advanced hip joint arthrosis, and recently underwent left hip arthroplasty.
On clinical examination, there is localised pain and tenderness in the region of the left ischial tuberosity and pain with all hip movements, on sitting and with straight leg raising.
On MRI, there are dual pathologies. There are features suggesting ischiofemoral impingement which is acute on chronic. The acute component is characterised by oedema in the quadratus femoris muscle and flattening or compression. The chronic component is characterised by muscle fatty atrophy. A reduced ischiofemoral space (between medial cortex lesser trochanter and lateral cortex ischial tuberosity ≤15mm) is contributory to the diagnosis.
There is also tendinopathy of the hamstring enthesis (conjoint tendon and semimembranosus) at the ischial tuberosity, and a tear of the adjacent adductor magnus from the inferior aspect of the tuberosity (called the ischiocondylar or “hamstring” component of the adductor magnus). The adductor magnus is sometimes considered a part of the hamstring complex and is uncommonly torn.
Patients with ischiofemoral impingement typically present with buttock pain and a snapping sensation exacerbated by a long duration of weight bearing or hip extension/adduction. In some cases, the sciatic nerve may be irritated, manifesting as neurological symptoms radiating to the leg and foot.
A “long-stride walking test” can be used to test for ischiofemoral hip impingement. A positive test involves a patient walking with a long stride and experiencing buttock pain lateral to the ischium during hip extension, with pain absent when walking with short strides.
Conversely, symptoms arising from hamstring tendinopathy typically originate from the ischial tuberosity, radiating to the posterior thigh, aggravated by prolonged sitting, with palpable tenderness in this location.
There are numerous factors predisposing to ischiofemoral impingement including:
- changes in alignment such as coxa valga, hip dysplasia, post-trauma or iatrogenic (e.g. post hip arthroplasty)
- masses
- intertrochanteric fracture
- valgus osteotomy
- medial implant offset after total hip arthroplasty
- excessive femoral neck anteversion.
Conservative therapy with analgesics or cortisone injection is the treatment of choice, with surgical options reserved for failed conservative management.
Dr Sebastian Fung is a musculoskeletal radiologist who undertook an MRI imaging fellowship in Hospital for Special Surgery in New York. He works in Sydney at St Vincent’s Private Hospital and Mater Hospital.
Fig 1a: Axial STIR image through the ischial tuberosity showing left sided narrowing of the ischiofemoral space and oedema (high signal) in the quadratus femoris muscle (red arrow). Adjacent is the tendinopathy of the hamstring origin tendons (blue arrow).
Note the normal appearance of the ischiofemoral space and quadratus femoris on the right (yellow arrow).
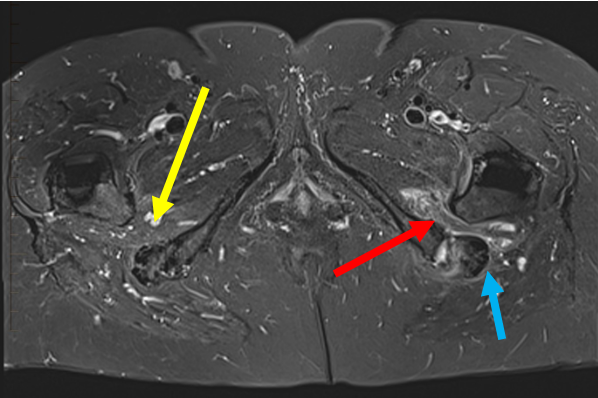
Fig 1b: Axial PD images showing fatty atrophy of the quadratus femoris and narrow ischiofemoral space (arrow)
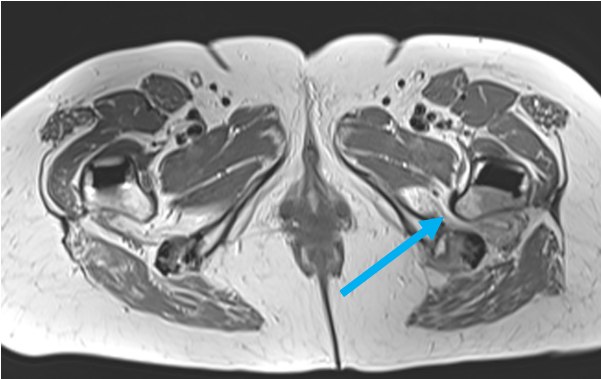
Fig 2: Axial STIR image immediately distal to the ischial tuberosity showing a tear of the left adductor magnus, which is sometimes considered a part of the hamstring complex (blue arrow). Note the low signal normal appearance of the right adductor magnus (yellow arrow).
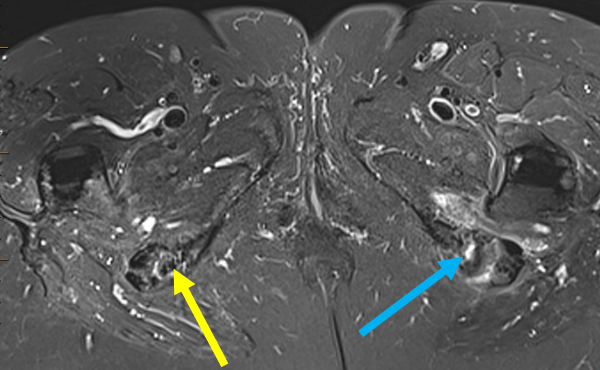
Fig 3a, 3b: Coronal images showing the adductor magnus tear (blue arrow). Degenerated, but not torn, semimembranosus and conjoint hamstring tendons are indicated with red arrows.
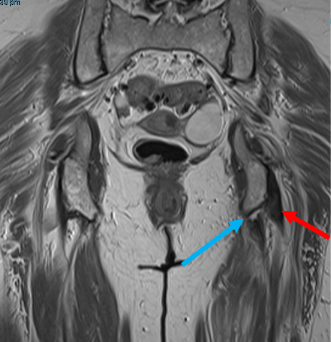
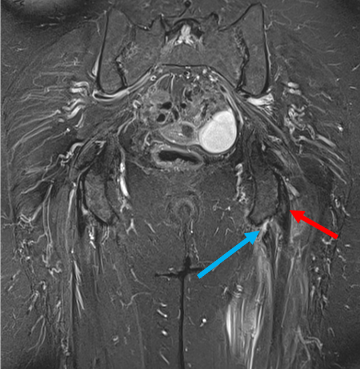
Fig 4: Frontal pelvic x-ray showing narrowing of the ischiofemoral space prior to hip arthroplasty.
PUBLISHER: Needs canonical from RR